
by Specialdocs Consultants | Jan 17, 2023 | Patient News
The First Hundred Years: Healthy Longevity May Ultimately Define the Future
Humankind has eternally searched for the fabled fountain of youth. While we suspect that a magical elixir to turn back time may never be discovered, in 2023 we are coming ever closer to a more achievable goal: using scientific breakthroughs to slow the process of aging and therefore prolong our healthspan. As the number of Americans celebrating their 90th, 95th and even 100th birthdays continues to rise, aging research has radically shifted from efforts to extend the lifespan to enhancing function and years lived independently. Countless studies, encompassing everything from launching stem cells into space to investigating the genetics of “super agers”, are underway. Below we explore some of the newest thinking and exciting breakthroughs to come with nationally recognized expert George Kuchel, MD, whose decades of successful research both at the bench and in clinical settings have contributed to shaping a new vision of how we age.
“We can’t reach old age by another man’s road. My habits protect my life but they would assassinate you.” – Mark Twain, 1905
Individuality in Aging
“We used to look at older adults as if they were all the same, with everyone becoming old the day they retired at 65,” says Dr. Kuchel, director of the UConn Center on Aging, which was established in 1985, making it one of the first multidisciplinary centers focused on improving the lives of older adults through research, education and clinical care. “While aging is inevitable and a normal part of the lifespan process, there’s tremendous heterogeneity, or variability, in how each of us ages. When we study the rate at which individuals age in terms of physical and cognitive function, frailty, disability, and disease development, we find increasing heterogeneity with age. Therefore, rather than focusing on averages typically culled from observational studies of older people compared to younger people, we are focusing on the differences within those averages.”
Geroscience and Aging Adults
Better understanding the uniqueness of each individual as they age has inspired Dr Kuchel and his colleagues to spearhead the burgeoning new field of Precision Gerontology. The overarching goal is to develop treatments for older patients that are more effective in promoting health and independence by being more precise and targeted. Adding exponentially to this knowledge base is the field of Geroscience, which seeks to delay the onset and progression of different chronic diseases by targeting the shared biological mechanisms that make aging a major risk factor and driver of common chronic conditions and diseases of older people.
“Many older people have multiple ongoing chronic conditions, and see different physicians for each,” says Kuchel. “However, as geriatricians and concierge medicine physicians were among the first to recognize, looking at the whole patient is essential. Geroscience transforms the ‘one disease at a time’ approach by studying the role of biological aging in enabling all these conditions.”
The 2021 launch of the NIA Older Americans Independence “Pepper” Center at UConn, one of only 15 National Institutes of Health (NIH)-funded centers across the country dedicated to enhancing function and independence in older adults through research, has significantly advanced the scope of studies at the university. According to Kuchel, “We are combining evidence-based geriatric care with more individualized treatments involving emerging interventions designed to delay the onset of chronic diseases by targeting biological aging. Our work moves us closer to the mission of extending the healthspan of greater numbers of individuals.”
Studies Related to Healthy Aging and Longevity
Promising studies under the microscope at UConn and other prominent research institutions include:
Can chronic diseases be delayed by targeting aging?
A geroscience-based trial to test the effectiveness of diabetes drug metformin in slowing the onset of chronic diseases in older adults is slated to be announced in 2023. The randomized, six-year TAME (Targeting Aging with Metformin) trial, led by the American Federation for Aging Research, will engage over 3,000 individuals nationwide between the ages of 65 and 79 to test if those taking metformin experience decreased or delayed onset or progression of age-related diseases such as cardiovascular disease, cancer and dementia.
Dr. Kuchel believes that conducting the trial will prove revolutionary. “Metformin has an excellent safety profile, proven over more than six decades,” he says, “and uniquely among other oral hypoglycemics, it appears to have a broad effect on many aspects of aging.” By collecting and analyzing trial participants’ serum, plasma, blood, urine and stool for varied biomarkers, the study will also provide information about a person’s risk of developing a disease, and lay a solid foundation for future biomarker discovery and validation as well as accelerating the pace of geroscience research.
Worth noting: In earlier stages is the study of rapamycin, an immunosuppressant currently used in high doses in transplant patients. However, when used in much lower doses the drug promotes longevity and reduces age-related disease in animal models, while it improves influenza vaccine responses in community-dwelling older adults.
Senolytics
This entirely new class of drugs may one day be used to halt cellular senescence, a hallmark of aging. As cells age and lose their ability to divide, they secrete molecules that trigger inflammation and cause much of the damage seen in osteoporosis, arthritis, diabetes, sarcopenia, cardiovascular disease and cancers. In numerous animal trials, use of senolytic drugs such as fisetin to selectively eliminate and clear senescent cells from the body were shown to significantly improve function. Multiple placebo-controlled, double-blind studies with older patients are planned or underway through the National Institute of Aging Translational Geroscience Network and elsewhere.
Inside the microbiome
This topic of intense interest continues to build an impressive body of research, including a recently completed collaboration between UConn Center on Aging and Julia Oh, PhD, at the Jackson Laboratory for Genomic Medicine on the same campus. This study showed the presence of an altered microbiome (the millions of microbes living in our gut, mouth, skin and elsewhere) in nursing home residents. Importantly, the changes were specific to frailty rather than biological age, and linked to bacteria associated with severe infections and antibiotic resistance. Going forward, in keeping with a focus on Precision Gerontology, clinical approaches may be used to identify individuals with high risk for severe infections and to explore treatments for restoring the microbiome to a state characteristic of younger or less frail individuals.
Personalized influenza vaccines
Another example of Precision Gerontology research is underway with Duyu Ucar, PhD, at the Jackson Laboratory and the Icahn School of Medicine at Mount Sinai, studying adults aged 65 and older over the next three influenza seasons to pinpoint the age-related immune alterations that reduce influenza vaccine effectiveness. “We know the body’s ability to produce a robust immune response after receiving the flu shot decreases with age, and we’ll be testing whether next-generation influenza vaccines, including mRNA-based ones, can help boost these immune responses. Understanding the factors that predict good responses to each vaccine will allow us to ultimately personalize our recommendations,” explains Kuchel.
“This is truly a time of meaningful change and ongoing advances in the field of aging,” says Kuchel. “Each day we uncover new answers to the question that has inspired our research from the start: ‘How can we add life to our years?’”

by Specialdocs Consultants | Jan 17, 2023 | Healthy Aging, Patient News
The growing group of people able to enjoy 100 years of life may well be one of the most remarkable achievements of the 21st century. A generation ago, the number of centenarians worldwide was just 110,000; today they are 600,000 strong. Notably, a sizable segment of this long-lived group, aptly called Super Agers, reach 100 in good health with no age-related disease or disability. Are they the fortunate recipients of outstanding genes, followers of a particularly healthy lifestyle, or a combination of both?
Definitive answers may start to emerge sooner than we had imagined possible, thanks to the SuperAgers Family Study, called one of the most ambitious ever conducted, with the goal to uncover and understand the genetic and biological mysteries of exceptional longevity and healthy aging. The initiative, spearheaded by the American Federation for Aging Research (AFAR) and Albert Einstein College of Medicine, in collaboration with https://www.bumc.bu.edu/busm Boston University School of Medicine, will recruit 10,000 people over age 95 to collect their DNA samples and health histories, as well as their children’s.
“Super Agers show us that chronic disease is not an inevitable part of aging, and that an extended period of good health can accompany a long lifespan,” says Sofiya Milman, MD, principal investigator of the study and director of Human Longevity Studies at Einstein’s Institute for Aging Research.
While previous research has attempted to pinpoint the distinctive characteristics of people living well in their ninth and tenth decades, the enrollment of 10,000 participants in SuperAgers will represent the largest cohort ever studied. The extensive numbers are essential to obtaining meaningful data that can benefit many in the future, according to Milman.
“We believe longevity may be linked to rare genetic variants found in less than five percent of the population, making it a challenge to amass ample genetic evidence,” explains Milman. “The enormous data bank being built in our SuperAgers study will enable us to identify these genes, understand their biological pathways and explore how to duplicate their functions.”
Milman aims to achieve full enrollment over the next two to three years, with results from the first phase available in 2024. “SuperAgers will significantly accelerate our research by providing us with a treasure trove of data on not just genetics, but biological and behavioral factors that affect aging and its related diseases. Ultimately, this will help us develop, trial and fast-track new therapies to extend a healthy old age,” she says.
In the meantime, adhering to a nutritionally balanced diet, exercising, getting sufficient sleep, managing stress and eliminating tobacco are all well advised. “A healthy lifestyle alone may not be enough to guarantee you reach 100,” admits Milman, “but all evidence points to the fact that it will extend your healthy lifespan.”
SuperAgers Sign-Up
Interested in being part of the SuperAgers family study?
Individuals who have passed their 95th birthday, as well as children of those individuals, are invited to enroll online at http://www.superagersstudy.org and complete a health history, family history and demographic profile. Those eligible will receive a biospecimen collection kit in the mail and are asked to return it in a postpaid envelope to the Albert Einstein College of Medicine, which will store and process each participant’s DNA. Please note that participants may choose to receive results regarding their ancestry or family origins. The SuperAgers biobank holding the DNA records, and all the related data, will be protected and maintained at Einstein in compliance with federal medical privacy law (HIPAA).


by Specialdocs Consultants | Oct 6, 2022 | Healthy Aging, Patient News, Wellness
Senior Moments Or Something More?
As Baby Boomers continue the inexorable journey deep into their senior years, preserving cognitive function understandably tops the list of worries. While Alzheimer’s Disease and related dementias are seen in just 5% of people over 65, that number jumps to 30% for people age 85 and over. Questions abound: is forgetting a name a sign of normal aging or an indicator of a more serious memory disorder? Are any nutritional supplements or pharmaceutical treatments available that are proven to stave off memory loss? Most importantly, what steps can be taken to modify individual risk?
To better understand how to identify and manage dementia and Alzheimer’s disease, we asked one of the country’s leading experts, R. Sean Morrison, MD, for his informed perspective on this growing concern for seniors, their families and caregivers. A practicing geriatrician, palliative medicine physician and health researcher for almost three decades, Dr. Morrison has earned numerous awards and recognition for his work, and currently serves as the Chair of the Brookdale Department of Geriatrics and Palliative Medicine at the Icahn School of Medicine at Mount Sinai and as Director of the Hertzberg Palliative Care Institute.
 Is memory loss an inevitable, natural sign of aging?
Is memory loss an inevitable, natural sign of aging?
Dr. Morrison: The good news is that not all cognitive functions decline with age. The ability to maintain attention, language comprehension, usage, and vocabulary does not decrease. Knowledge learned years ago like how to ride a bike, or brush your teeth, also stays intact. Additionally, when you learn something new and can remember it, you won’t forget it any more rapidly than when you were younger.
The not so good news is that it will take greater effort to learn those new things; more attention, repetition and use of memory-enhancing strategies will be needed. The ability to multitask is also diminished, as processing information takes longer and reaction times are slower. People may experience poorer performance when working under time pressure, and find it more difficult to manipulate information in the brain, such as calculating a tip in a restaurant or figuring out a route to travel from one place to another.
 How do you distinguish between a “senior moment” lapse in memory and a sign of Alzheimer’s disease?
How do you distinguish between a “senior moment” lapse in memory and a sign of Alzheimer’s disease?
Dr. Morrison: So many people experience that temporary inability to remember a name. But if you are able to recall things with a cue or can pick it out from a list of possibilities, that’s evidence of a problem with retrieval but not with storage. You can be reassured that it doesn’t indicate Alzheimer’s disease but a “senior moment” because the information has been successfully stored in your memory.
 Is routine screening for dementia recommended in older adults?
Is routine screening for dementia recommended in older adults?
Dr. Morrison: The U.S. Preventive Services Task Force does not recommend for or against routine screening, saying no interventions are proven to have a significant effect in people with earlier detected cognitive impairment. However, it is required as part of Medicare’s yearly assessments, and most primary care physicians consider dementia screenings an essential part of their annual wellness exam.
 What types of screening tests do you recommend?
What types of screening tests do you recommend?
Dr. Morrison: At least a dozen tests are available, each with their own benefits and drawbacks. I recommend the following for their ease of use and proven sensitivity and specificity in diagnosing cognitive impairment:
- Mini-Cog is a quick, three-minute evaluation. Patients are asked to repeat three words, draw a clock with hands at a specific time, and then recall the initial three words.
- Memory Impairment Screen assesses free and cued word recall. Patients are read four unrelated words from four categories (e.g. Red Cross, saucer, checkers, telegram) and after a few minutes of diversion, asked to recall the words in 20 seconds, either with no prompting or cued by category.
- Animal Fluency Test. Patients are asked to name as many animals as possible in a 60-second period.
 Are there any risk factors for dementia and Alzheimer’s disease that can be controlled by patients?
Are there any risk factors for dementia and Alzheimer’s disease that can be controlled by patients?
Dr. Morrison: Quite a few risk factors are modifiable with lifestyle changes and non-pharmaceutical treatments. These include:
- Address hearing and visual impairments, with eyeglasses, hearing aids and other assistance
- Prevent and manage hypertension and diabetes
- Maintain a healthy weight
- Stop smoking
- Seek treatment for depression
- Prioritize regular exercise and physical activity
- Avoid social isolation
- Explore cognitive training
The best advice I can give to people in their 50s to 70s looking to prevent or delay progression of dementia and Alzheimer’s disease: exercise, exercise, exercise and rigorously control your blood pressure.
 How are the symptoms frequently experienced by people with dementia – sleep disturbance, mood disorders, agitation – best addressed?
How are the symptoms frequently experienced by people with dementia – sleep disturbance, mood disorders, agitation – best addressed?
Dr. Morrison: There are a number of non-pharmaceutical interventions that have proven effective. Use adaptive clothing and assistive devices to help eliminate distress around bathing and dressing. Create a reassuring familiar structure to the day with a regular routine and activities. Optimize the sleep environment with a comfortable temperature, the right amount of light, a warm milky drink and a bath or shower before bed; avoid stimulating medications, drinks containing caffeine and alcohol, and exercise too close to bedtime. Pharmaceutical treatments can also be considered, including antidepressants to improve cognition and ameliorate agitation and aggression, and melatonin and melatonin antagonists to help with sleep disorders. Of note: medications such as benzodiazepines (BZD), non-BZD hypnotics, mood stabilizers and antipsychotics are no longer routinely recommended as side effects can outweigh possible benefits.
 Are there any benefits to nutritional supplements or appetite stimulants?
Are there any benefits to nutritional supplements or appetite stimulants?
Dr. Morrison: Nutritional supplements can help with weight gain in patients with anorexia or cachexia (‘wasting’ syndrome) but have no meaningful impact on survival. And while appetite stimulants such as cannabinoids and steroids are often given to help patients with dementia, there is no consistent data regarding their safety and efficacy.
 What medications are available to treat or stop the progression of dementia?
What medications are available to treat or stop the progression of dementia?
Dr. Morrison: Until last year, only four medications were approved for treatment of dementia and Alzheimer’s disease, showing only a minimal to modest improvement in cognition. In 2021 a fifth drug was launched – aducanumab – a monoclonal antibody designed to reduce amyloid protein in the brain. Its fast-track approval was quite controversial as the clinical benefits of the drug were not proven during trials, which were stopped early as a result, and some severe side effects were observed. Interestingly, some researchers are now rethinking the idea that targeting amyloid protein plaques will eliminate Alzheimer’s disease, and instead exploring Alzheimer’s as a disease of inflammation. This could be the next fascinating line of research.
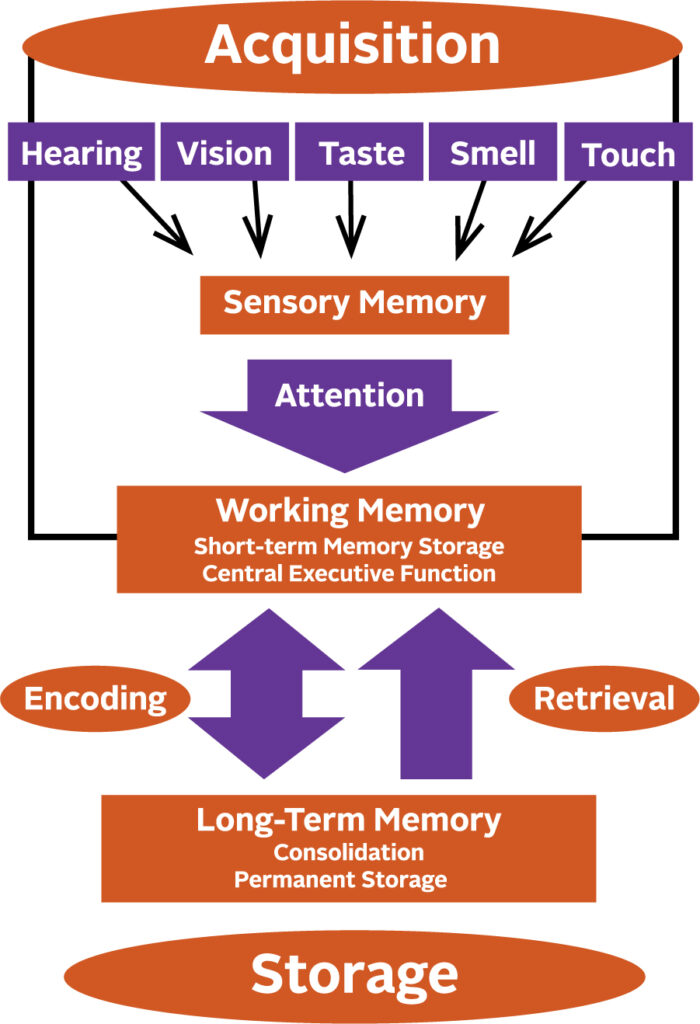
How a Memory is Made
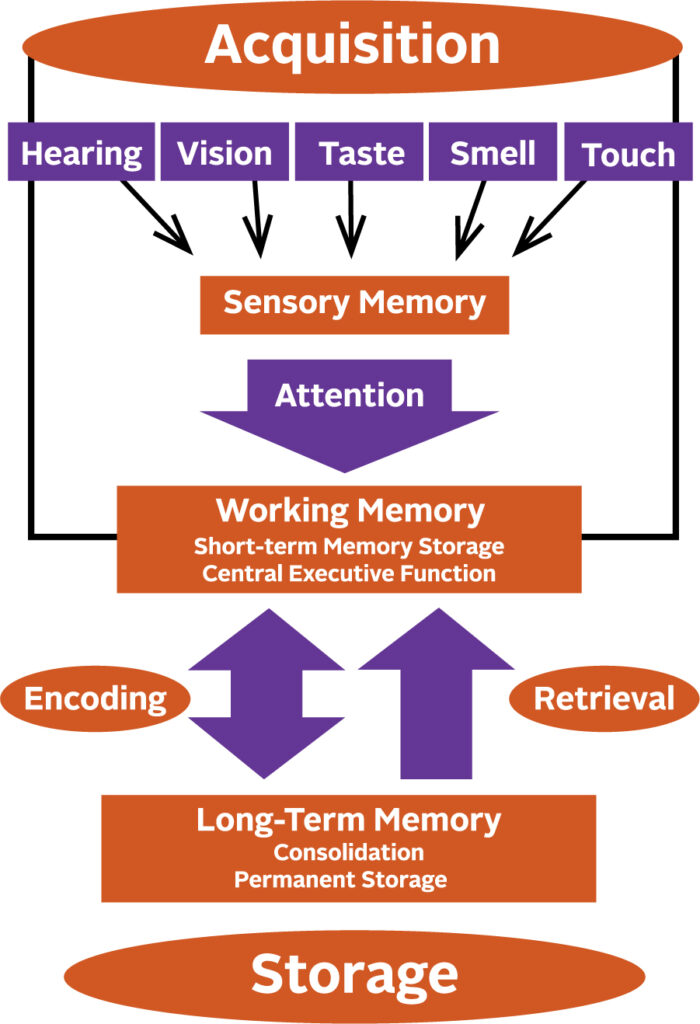
Memory begins to form by giving attention to the information received through your senses. Anything that interferes with your ability to pay attention, such as hearing impairment, will affect the formation of a sensory memory. Successful integration of sensory memories into your working memory enables you to temporarily store, organize and manipulate information. These memories are then encoded into long-term memory and finally put into permanent storage.

by Specialdocs Consultants | Oct 6, 2022 | Nutrition, Patient News
Mindful Eating for Your Brain
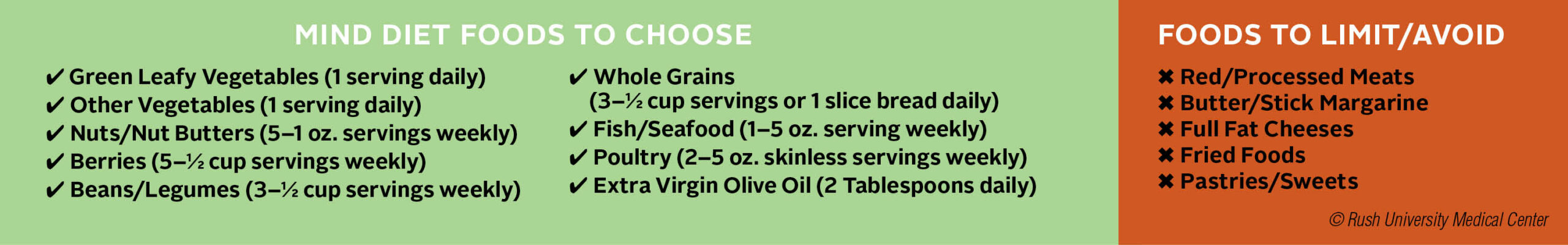
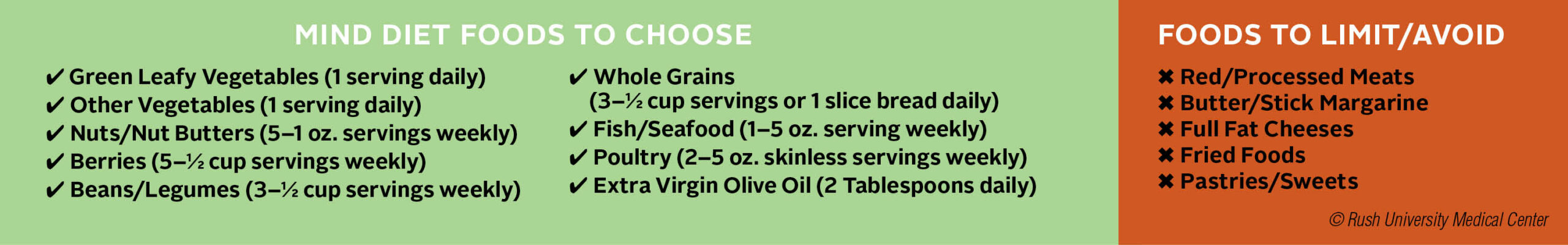
Harkening back to ancient civilizations, the concept of food as medicine represents one of today’s most cutting-edge approaches to prevention and disease management. Inspired by the intricate connection of mind and body wellness, a small, special group of diets have made their way into the mainstream offering benefits far beyond short-term weight loss. Among them are DASH (Dietary Approaches to Stop Hypertension), a low-sodium diet that encourages consumption of foods rich in nutrients such as potassium and calcium and magnesium; the Mediterranean diet for heart health, emphasizing fish, fruits, and vegetables, with olive oil as the main source of fat; and combining both, the MIND (Mediterranean-DASH Intervention for Neurodegenerative Delay) diet, which shows real promise in helping its adherents preserve cognition and reduce the risk of dementia.
Launched in 2015 by researchers at Rush University Medical Center, the MIND diet encourages selecting foods from categories that include leafy greens and vegetables, legumes, fish and seafood, poultry, nuts and berries, while limiting high fat, high sugar and processed foods. Longitudinal observational studies showed the rewards of shifting to this healthier way of eating, with a 53% reduction in the risk of dementia for seniors who rigorously followed the diet, and somewhat surprisingly, a 35% risk reduction even for those who followed it only moderately well.
“This is my favorite feature,” says Jennifer Ventrelle, MS, RD, lead dietitian for the MIND Diet Intervention to Prevent Alzheimer’s Disease at Rush, “you don’t have to be perfect! It’s not necessary to eat from every preferred category to achieve your goals.”
Although it’s not intended as a reducing diet, Ventrelle says people who follow it naturally lose weight by focusing on the preferred categories of foods. “It’s too difficult for many people to consider banishing all sweets or giving up red meat forever, so we haven’t eliminated these foods but allow them with limited frequency and close attention to portion sizes,” she explains.
Additional research pointed to a host of other benefits associated with eating MINDfully for older adults: slower cognitive decline and progression of Parkinsonian signs in aging, and reduced risk of functional disability, depressive symptoms, metabolic syndrome, cardiovascular disease and all-cause mortality. “The literature continues to grow, with new studies that point to the key role diet plays in preventing cognitive decline,” says Puja Agarwal, PhD, nutritional epidemiologist and assistant professor of internal medicine at Rush.
But it is the gold-standard randomized controlled trial begun several years ago by Rush and Harvard School of Public Health that may ultimately establish a causal relationship between diet and dementia. More than 600 participants at higher risk for Alzheimer’s disease – overweight, suboptimal diets and a history of dementia in the family – were enrolled in the study designed to directly measure whether following the MIND diet versus a low-fat diet can prevent neurodegenerative ills – results are expected by the end of 2022. According to Agarwal, who is fully aware of its significance at a time when more than 6 million people in the U.S. are living with Alzheimer’s disease, a number expected to double in the coming decades. “We don’t have a cure for these diseases, so prevention strategies are essential. We’re hoping for intervention trial results for the effect of MIND diet in protecting the brain to further establish the role of diet in healthy aging.”
What a day of meals on the MIND diet might include*:
BREAKFAST
Greek Yogurt Parfait: ½ cup whole grain, high fiber cereal, ½ cup berries, ½ cup low-fat Greek yogurt, 2 tbsps (raw, unsalted) walnuts, almonds or pecans.
LUNCH
Whole Wheat Turkey Wrap: 1 tortilla wrap + 3-5 oz turkey breast lunchmeat or carved white meat + 1 slice reduced fat cheese + lettuce, tomato and veggies of choice.
3-Bean Salad: Mixture of kidney beans, black beans, chickpeas, red onions + 1 tbsp extra-virgin olive oil + 1 tsp balsamic vinegar + Italian seasoning mix such as oregano, parsley, basil, etc.
SNACK
Mediterranean Rice Cake: 1 whole grain rice cake spread with 2 tbsps hummus topped with cucumber slices, tomato slices + fresh lemon juice.
DINNER
Baked Salmon over Spinach and Grains with Asparagus
- 3-5 oz salmon filet topped with fresh or dried dill or parsley + a squeeze of fresh lemon juice baked on top of 1 cup baby spinach leaves
- 8 asparagus spears topped with ½ tbsp extra-virgin olive oil + fresh lemon juice + zest
- 1 cup cooked whole grain such as brown rice, quinoa, or bulgur mixed with ½ tbsp. extra-virgin olive oil
DESSERT
1 oz of dark chocolate (at least 75% cocoa) and ½ cup frozen berries
*Please consult with your physician to determine if these foods are appropriate for you.

by Specialdocs Consultants | Jul 8, 2022 | Healthy Aging, Patient News, Staying Active
Try Pickleball, the Country’s Fastest-Growing Sport
Tired of the same ‘ole routine every summer but find yourself in a pickle and looking for a new summer activity? Well, according to American Council on Exercise (ACE), you might want to consider pickleball.
As everyone from your next-door neighbor to ACE will attest, pickleball is extraordinarily popular. Its rapid rise to ubiquity can be attributed to a number of factors, ranging from easily learned rules and minimal equipment needs to intergenerational appeal and abundant opportunities for socializing.
This blend of badminton, tennis and table tennis can be adjusted to suit the intensity and competitiveness of the players, making it simple enough for beginners but fast-paced enough for more fit or skilled participants.
All of which is to say that if you haven’t yet considered picking up a pickleball paddle and the light, whiffle-like plastic ball, summer 2022 might be the perfect time to do so.
“Pickleball doesn’t require the skill of tennis, so it is easily adapted by most, and provides all the benefits of movement, including calorie burning and enhanced functional capabilities,” says Dr. Cedric Bryant, ACE president and chief science officer.
Already a favorite sport in retirement communities, pickleball has swelled to include more than 4.8 million players in the U.S. – almost double the number from five years ago – earning it the title of fastest-growing sport in 2021 and 2022. According to the Sports and Fitness Industry Association, the spike has been fueled by people ages 54 and younger looking for a friendly yet competitive and lively sport.
“People who play are generally having so much fun they don’t realize how much exercise they’re actually getting,” says Laura Gainor, spokesperson for the USA Pickleball Association.
At 44 x 20 feet, the pickleball court is one quarter the size of a tennis court, so it’s easier to keep the ball in play and achieve a brisk workout. According to ACE, pickleball may provide just what many middle-aged and senior adults are seeking – a safe and effective workout that yields long-term benefits and encourages lifelong participation.
A small research study recently conducted by the organization among people ages 40 to 85 showed that playing four 15-minute pickleball matches three days each week meets exercise intensity guidelines for improving and maintaining cardiorespiratory fitness. Study authors reported the positive impact on cardiometabolic risk factors, with participants experiencing favorable changes in cholesterol levels, systolic and diastolic blood pressure, and peak oxygen uptake after six weeks.
The smaller court also benefits older people or those who have problems with their joints, because less running is needed, resulting in less wear and tear on the joints. One cautionary note: Experts advise learning proper technique to prevent falls. As always, be sure to check with your healthcare provider before beginning any new physical activity.
“Take a few lessons to get started, and you’ll quickly ramp up,” assures Gainor. “After three to five games, you’ll have a very good understanding of how to play, and will become addicted to it shortly after!”
Take It Outside: Keep Moving This Summer
There’s no one-sport-fits-all approach, so if pickleball doesn’t appeal, find your inspiration in one of these activities, spanning the spectrum from low exertion to highly energetic:
- Stroll through farmers’ markets or art fairs
- Go produce picking at a local orchard
- Forest bathe – immerse yourself in nature at a forest preserve
- Gardening – remember to bend from your knees and waist rather than your back
- Swim – use a variety of strokes to limber up your whole body
- Disc golf – a low-impact way to challenge your coordination
- Yard yoga – take your mat and routine outdoors
- Hike, jog, run or cycle on an outdoor trail
- Kayaking – for a vigorous upper body workout
- Stand-up paddleboarding or Boga – challenging, board-based water workouts
Sources: American Council on Exercise, American Heart Association, USA Pickleball Association

by Specialdocs Consultants | Jul 8, 2022 | Patient News, Wellness
Stay Safe with Sunscreen, Sunglasses and Plenty of Water
The longer, sunshine filled days of summer are upon us and without a doubt, they are one of life’s unrivaled joys, especially when you protect yourself from the powerful impact of ultraviolet rays. With that in mind, we share our tips for safe summer fun; from choosing and using the right sunscreen to staying hydrated.
The debate around sunscreen safety heated up with last year’s recall of some popular consumer products containing chemicals such as benzene, which is absorbed through the skin and into the bloodstream. Yet according to the FDA, the American Academy of Dermatology and other experts, there is minimal evidence that systemic absorption of these ingredients is toxic or harmful to health. There is, however, a mountain of proof regarding the harmful effects of sunburn – most notably its significant contribution to the risk of melanoma.
“Use of a broad-spectrum, SPF 30 sunscreen effectively blocks UVB and UVA rays to prevent sunburn,” says Dr. Andrea Murina, MD, associate professor of dermatology at Tulane University School of Medicine and director of the University Medical Center’s dermatology clinics. “This not only reduces the risk of developing skin cancer but also decreases signs of early aging on your skin (such as wrinkles, age spots, sagging skin) and stops existing melasma from darkening and new patches from appearing.”
According to Dr. Murina, while we know some ingredients in sunscreen do cross over into the bloodstream, most are rated by the FDA as GRASE, meaning generally recognized as safe and effective.
A bit of background: Earlier studies conducted by the FDA showed that common chemical ingredients used in sunscreen, including oxybenzone are absorbed into the bloodstream.
Further research on whether systemic absorption of oxybenzone was an actual concern was suggested. However, no clear links to any health problems in humans were identified.
Nevertheless, the ingredient has been eliminated from most sunscreens currently being manufactured, making it easy to find an oxybenzone-free product.
When applied correctly, a water-resistant, SPF 30 sunscreen is optimal, blocking 97% of UVB rays. “A higher SPF is fine, but only incrementally blocks more rays, and the time and duration of effectiveness is the same,” says Murina.
The best way to protect yourself is by using a combination of measures:
- Wear sun-protective clothing, including a lightweight, loose-fitting, long-sleeved shirt, pants, a wide-brimmed hat and sunglasses. Darker colors, densely woven cloth, unbleached cotton and shiny polyesters are recommended by the Skin Cancer Foundation.
- Judiciously apply broad-spectrum sunscreen every two hours on uncovered body parts, such as top of hands, face, neck and ears.
- Swap out regular SPF 15 foundation for a tinted sunscreen. “There are so many cosmetically elegant ones available today that mimic the look of makeup but offer much more protection,” says Murina. Tinted sunscreens with an SPF of 30 or higher provide protection that blends well with all types of natural skin tones, and help prevent exposure to both UV rays and visible light from the sun.
- Seek shade when the sun’s rays are strongest, between 10:00 a.m. and 2:00 p.m.
Like sunscreen, sunglasses are vital in blocking the harmful effects of UV radiation. UVA and UVB rays can cause increased risk of conditions such as cataracts, eye cancers and growths on the eye, as well as premature aging of the delicate skin around your eye. Choose sunglasses that block 99% or 100% of all UV light or are listed as having UV absorption up to 400nm. Wear them even when it’s hazy or cloudy, as UV light can pass right through clouds. And although you’ve undoubtedly heard this piece of advice before, it bears repeating: To protect your retina, never look directly at the sun.
Finally, drink up when you’re out in the sun. Water is the elixir of choice, helping to lower your body temperature and replace the fluids you lose through sweating. This is particularly important for older adults whose body’s fluid reserve becomes smaller and thirst sense decreases as they age. Be aware of the most common signs of dehydration – lightheadedness, fatigue, dizziness, less frequent urination, dark-colored urine – and rehydrate promptly with cool water.
Safe Travels
If your summer vacation includes international travel, we recommend some healthy pre-planning that includes the following:
- COVID-19: Make sure you are up to date with your vaccines and boosters. Get tested for COVID-19 as close to the time of your departure as possible (no more than three days before travel). Do not travel if you have COVID-19 symptoms, if you tested positive or if you are in quarantine due to possible exposure.
- Check the U.S. Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO) websites for the most up-to-date travel alerts, advisories and recommendations. Immunizations needed will vary based on your health condition, immunization history, countries and regions on your itinerary, and duration of your visit.
- Update your routine immunizations to protect against increased risk of exposure to illnesses such as seasonal flu, diphtheria, varicella (chickenpox), measles, mumps and rubella. For quick guidance on additional immunizations you may need, try the online tool at GlobalTravEpiNet.
- To protect yourself from the serious diseases spread by mosquitos, such as dengue fever and malaria, bring an EPA-registered insect repellent with an active ingredient like DEET or picaridin.
- Pack your prescription medications and consider bringing over-the-counter medicines, including anti-diarrheal medicine, antacid, antihistamine, hydrocortisone cream, motion sickness medicine, cough medicine, pain and fever medicine, and mild laxative.
- Also, pack supplies to prevent illness or injury, such as hand sanitizer, water purification tablets, insect repellent and sunscreen; and first aid items such as antibacterial ointment, antiseptic wound cleanser, aloe gel, insect bite cream, a digital thermometer and bandages.
We encourage you to contact your health care provider four to six weeks prior to your trip for personalized guidance … and we wish you a safe and memorable journey!
Sources: FDA, American Academy of Dermatology, Mayo Clinic, American Academy of Ophthalmology, U.S. Centers for Disease Control and Prevention, Skin Cancer Foundation








Recent Comments