
by Specialdocs Consultants | Apr 14, 2023 | Healthy Aging, Medical Conditions, Medications, Nutrition, Patient News
Except for dedicated thespians, saying “break a leg” is most definitely not a harbinger of good luck. More than 10 million Americans are living with osteoporosis, a condition of low bone mass that results in increased risk of bone fracture, sometimes even from a minor fall or pressure from a big hug. Over 1.5 million osteoporotic fractures occur annually, and 1/3 of women and 1/5 of men over 50 will experience an osteoporotic bone fracture in their lifetime. The good news is that reliable diagnostic testing and treatments are available, which we share below.
Who’s at Risk for Osteoporosis?
Osteoporosis is sometimes referred to as a “silent disease” because it is painless unless a fracture occurs, so people often are unaware they have it until that happens. Post-menopausal women are at highest risk, in part due to the decline in estrogen levels. Estrogen, and to an even greater extent, testosterone, are hormones that help ward off osteoporosis, which is why it is not as common in men. Others at risk include those with autoimmune diseases such as rheumatoid arthritis and celiac disease, those with high parathyroid or thyroid levels and certain other chronic diseases.
Medications including corticosteroids, proton pump inhibitors and certain antidepressants and anti-seizure medications may increase risk of bone thinning. Inherited factors may affect risk, such as race (more common in Caucasians and Asians), body shape and size (smaller/thinner individuals more at risk) and family history of osteoporosis. Physical activity level and diet play a role, placing those who are sedentary and/or have a diet low in calcium at higher risk. Cigarette smoking and higher alcohol intake are also risk factors.
How Osteoporosis is Diagnosed
A bone density measurement test is the best way to diagnose osteoporosis, using the DEXA (dual energy x-ray absorptiometry) scan of hip and spine. The severity of decrease in bone mass is determined by your T-score: Between -1.0 and -2.5 is defined as osteopenia, when bones are weaker than normal, while -2.5 or less indicates osteoporosis.
Osteoporosis Medications
A number of medications are available to treat osteoporosis.
- Bisphosphonates to slow the breakdown and removal of bone are typically tried first. Fosamax, used most, is a weekly pill often taken for 5 years followed by a “drug holiday.” The IV bisphosphonate Reclast is generally continued for three years.
- Evista is a daily pill for post-menopausal osteoporosis that protects against bone loss and also reduces the risk of breast cancer in high-risk women.
- Prolia is injected every 6 months to slow breakdown and removal of bone and help increase bone density. It should not be discontinued once started or must be followed by another medication if stopped.
- Evenity is injected once a month for a year to increase new bone and reduce breakdown and removal of bone.
- Forteo and Tymlos are drugs that help build bone for people at high risk of fracture. These are injected daily for two years.
Managing Osteoporosis
Peak bone mass is achieved by age 25-30 years, but at any age, a healthy lifestyle can aid in strengthening bones. Focus on eating a balanced diet rich in vitamin D and calcium (see sidebar), and remember that exposing the body to natural sunlight increases production of vitamin D. Eliminating tobacco use and limiting alcohol is strongly recommended to promote maximum absorption of calcium and vitamin D. Taking fall prevention measures is crucial: consider that 95% of hip fractures are caused by falls.
Aim for 30 minutes of weight-bearing and muscle strengthening exercises on most days:
- Walk or run on level ground or a treadmill
- Dance
- Climb stairs
- Lift weights without straining your back
- Sit-to-stand exercises: start with an elevated seat height, and progress to a lower chair as you get stronger
- Strengthen thighs: stand against a wall and slide down into a slight knee bend, hold for 10 seconds and repeat a few times
- Tai Chi: combines slow movements, breathing exercises, and meditation
Nourishment Know-How for Bone Health
For optimal bone health, a daily intake of 1200-1500 mg of calcium and 400-800 IU (international units) of Vitamin D is recommended for adults. In many cases, supplementation may be appropriate.
Selected sources with calcium and/or Vitamin D:
- Dairy products
- Calcium- and vitamin D-fortified foods and beverages (soy or almond milks, cereals, cheese)
- Dark green, leafy vegetables
- Fish such as salmon, trout, mackerel, tuna, sardines
- Egg yolks
- Sesame or chia seeds, figs, almonds
Fall Prevention Measures for Those with Osteoporosis Include:
- Avoid ladders, step-stools and roof work
- Eliminate tripping hazards like throw rugs, obstacles or cords on the floor
- Be careful around pets and leashes
- Use good lighting, night lights, update glasses and eye care to optimize vision
- Stay fit with regular strengthening and balance exercises
- Wear non-slip shoes
- Install handrails and grab bars in the bathroom
Every patient is unique…please check with your healthcare provider to discuss recommendations for prevention and treatment based on your individual health situation.
Sources: Arthritis Foundation, AAOS, Orthoworld, Cleveland Clinic, National Academy of Medicine (formerly Institute of Medicine), UpToDate, US Department of Agriculture, American College of Rheumatology.
by Specialdocs Consultants | Apr 1, 2022 | Medical Conditions, Patient News, Wellness
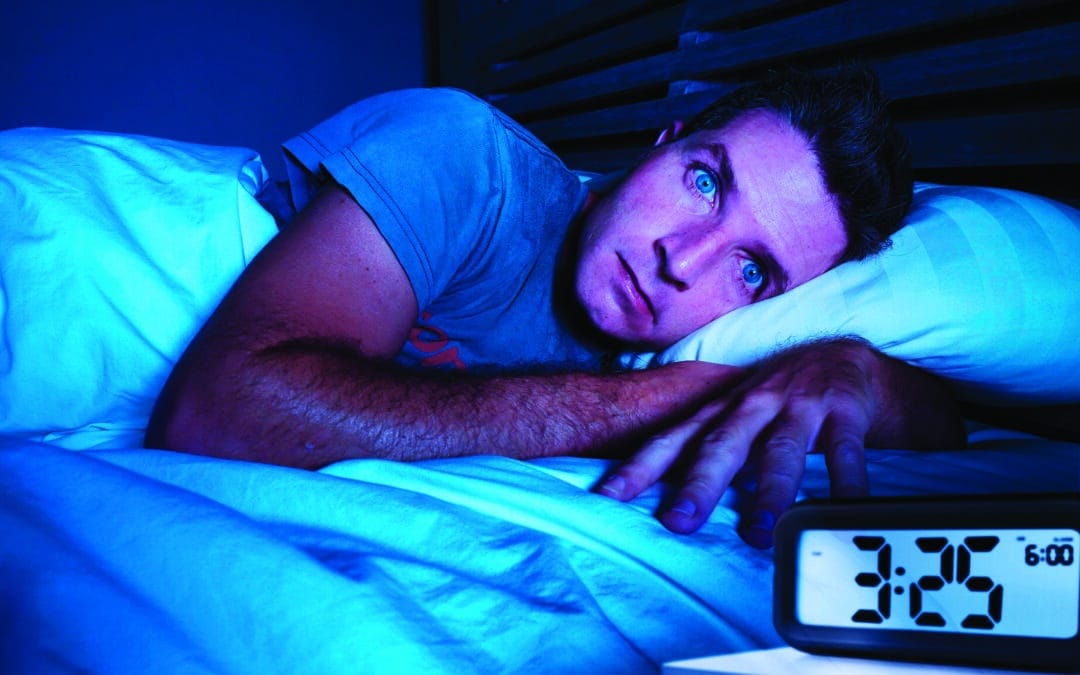
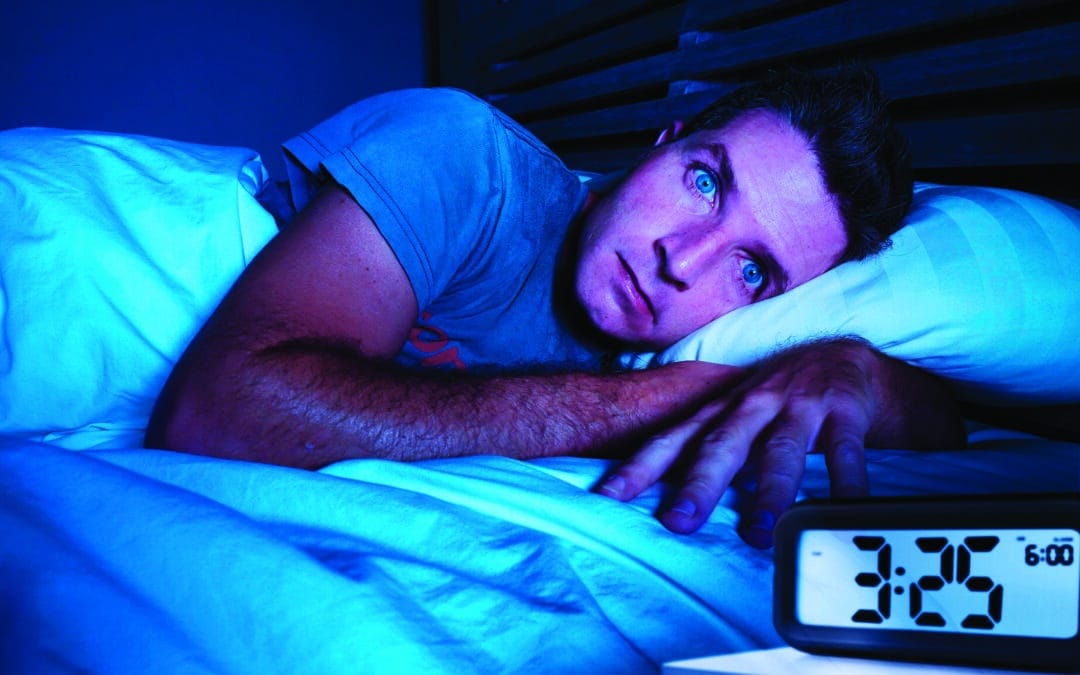
Breaking the Cycle of Anxiety, Insomnia and Sleep Anxiety
A good night’s sleep does more than refresh and revitalize. It’s essential to your health, so make it a priority to understand what’s keeping you up at night.
“Healthy sleep is as important as proper nutrition and regular exercise for our physical and mental well-being,” says Kannan Ramar, MD, sleep medicine physician at the Mayo Clinic’s Center for Sleep Medicine and immediate past president of the American Academy of Sleep Medicine. “Lack of sufficient sleep is associated with increased risks of type 2 diabetes, high blood pressure, cardiovascular disease, depression and anxiety.”
The sleepless nights and drowsy days previously experienced by one out of three Americans with insomnia rose to pandemic highs of almost 60% in 2021, sounding a wake-up call to address this treatable condition which profoundly impacts both mental and physical well-being.
Sleep disturbance is intricately interconnected with the presence of issues such as anxiety and depression, each influencing the others, so it’s not always possible to determine which came first. Behavioral changes that result from chronic insomnia include feelings of being overwhelmed, inability to concentrate, irritability, nervousness, restlessness, and a sense of impending danger or doom.
Of adults diagnosed with depression, 75% experience insomnia and 20% have obstructive sleep apnea. Similarly, anxiety can make it harder for the body to relax and fall asleep.
Research suggests that anxiety can also affect rapid eye movement (REM) during slumber and trigger vivid, disturbing dreams that wake the sleeper.
Completing the loop is sleep anxiety — apprehension or fear about going to sleep — which is commonly seen in those with insomnia, narcolepsy, sleep apnea or restless legs syndrome.
While insomnia can seem never-ending, a number of strategies can effectively break the cycle.
The Basics:
- Set boundaries for blue light exposure by turning off tv, tablets and phones at least 30 minutes before bedtime.
- Limit large meals, caffeine and alcohol within 3 to 4 hours of bedtime, which can disrupt sleep. Alcohol allows you to fall asleep quickly but not stay asleep throughout the night.
- Establish a consistent wake-up time seven days a week.
- Ensure your bedroom is a designated place of sleep by keeping it dark, cool and quiet. And turn around your clock so you can’t see the time if you’re tossing and turning in the middle of the night.
- Pursue support if you are experiencing chronic insomnia, defined as difficulty sleeping three or more times per week for at least three months. “We know that the longer insomnia lasts, the more difficult it is to treat,” says Dr. Ramar.
Support can include:
- Cognitive behavioral therapy for insomnia (CBTI), a form of talk therapy focused on learning how to create an optimal sleep environment with positive bedtime routines and avoidance of factors that trigger anxiety and negative thinking. Requiring up to 12 weeks to see results, the key is shifting from “trying hard to sleep” to “allowing sleep to happen,” according to Stanford Health.
- Prescription sleep hypnotics, such as Ambien or Lunesta. Hypnotics can be considered in conjunction with CBTI, but patients must be closely monitored for adverse effects and a buildup of tolerance to the medication’s effects. Low doses of Trazodone, an antidepressant, are sometimes used, as it causes drowsiness.
- Light therapy, which is especially helpful for those who need to reset their circadian rhythms; e.g., a night owl who wants to function better with an early morning rising time.
If you are experiencing too many wakeful nights, please let your healthcare provider know. It may be helpful to keep a sleep diary for several weeks to help pinpoint the habits affecting your ability to fall and stay asleep. In some cases, we may recommend a polysomnography (sleep study), where you’ll be monitored for blood oxygen levels, body position, breathing, electrical activity in the brain, eye and leg movements, heart rates and rhythms, sleep stages and snoring during an overnight stay in a sleep lab.
Finally, keep in mind that the amount of sleep needed per night – typically 7 or 8 hours on average – varies by individual. “If you function well and are fully alert during the day, you can be confident your sleep needs are being met,” says Dr. Ramar.

by lduque | Jan 11, 2022 | Medical Conditions, Patient News, Wellness
Coping With Sad This Winter
As we continue to weather the storm of COVID-19, seasonal affective disorder, or SAD, is once again on our radar. More subtle than an arctic blast, SAD is just as real, with just as much potential to have a chilling effect on our mood, productivity and wellness. Similar to last winter, the emotional stress and ongoing uncertainty that come with a global pandemic is unfortunately creating an ideal climate for SAD. Not surprisingly, mental health experts are expecting to diagnose and treat an increased number of people with SAD in 2022.
First discovered in the 1840s, SAD was not officially recognized as a disorder until the early 1980s, when Dr. Norman Rosenthal coined the term and categorized it as a form of clinical depression. We now know that SAD affects at least 5% of Americans; is more likely to affect women than men, those with other forms of depression or family members with the condition; and is far more common in northern regions, due to reduced natural sunlight. New research has advanced several theories as to why some people develop SAD, including: sluggish transmission of serotonin (which helps regulate mood and the body’s circadian rhythms; reduced sensitivity of the eyes to environmental light; a combination of these factors; or other reasons yet to be uncovered).
A deeper understanding of what triggers SAD and its impact on mental health has inspired a growing number of clinical treatments that can effectively neutralize its effects.
Chief among them:
Healing light.
Sitting in front of a bright light box for 30 to 45 minutes daily has been a treatment of choice for more than three decades, helping SAD patients with either 10,000 lux of white fluorescent or full spectrum light that shines 20 times brighter than ordinary indoor illumination. Dawn simulation, another form of light therapy, begins in early morning before patients awake by emitting a low level of light that gradually increases over 30 to 90 minutes to recommended room light level (approximately 250 lux). Enhancing indoor lighting with regular lamps and fixtures is also recommended).
Talk therapy.
Newer studies from the University of Vermont suggest that cognitive behavioral therapy (CBT), a psychological treatment aimed at providing patients with tools to change negative thoughts and behaviors, may be as effective as light therapy for treating SAD. According to the National Institute for Mental Health (NIMH), CBT adapted for SAD focuses on behavioral activation, helping SAD sufferers identify and engage in enjoyable seasonal activities to combat the ennui and fatigue they typically experience in winter.
Sleep hygiene.
Creating a consistent light-dark, sleep-wake cycle is important for SAD patients, who often experience hypersomnia (excessive daytime sleepiness) and insomnia (trouble falling or staying asleep).
Antidepressant medications. Because SAD is associated with disturbances in serotonin activity, antidepressant medications have been effectively used to treat symptoms.
Active days. Keep moving with daily walks outside, even on cloudy days, and aerobic exercise. Both can help alleviate symptoms of SAD.
Winterize your mental health
Be proactive in safeguarding your mental wellness over the coming months. Most importantly, know the symptoms of SAD and call our office for help if you’re experiencing:
- Diminished interest in things that were once enjoyable
- Low energy or overwhelming fatigue
- Difficulty with concentration or focus
- Worthless or helpless feeling
- Sleep issues: too much sleep, or not enough
- Changes in appetite or weight; increases in carbohydrate and sugar cravings
- Agitation
Experts advise those who’ve previously experienced episodes of seasonal depression to try to get in front of it this year. Call our office for guidance regarding medications or CBT sessions. For many, reprogramming their mindset can help restore proper circadian rhythms and eliminate the psychological dread of winter. Try enrolling in an online class, taking up a new hobby or creating a new routine to optimize daylight exposure. Or keep it even simpler. As Dr. Rosenthal told the New York Times, “A 20-minute early morning walk in the sun can be as good as commercial light therapy.”

by | Sep 11, 2021 | Medical Conditions, Patient News, Wellness
From Boosters & Breakthroughs to Vaccines & Variants: Where Do We Go From Here?
The following reflects an 8/24/2021 discussion; please check the CDC website for real-time updates as the situation continues to evolve.
Their answers may not land lightly, but epidemiologist Jodie Guest, PhD, and drug development expert Michael Kinch, PhD, have been immersed in examining COVID-19 since its first stirrings in early 2020. They share an informed look at the road ahead for us all.
State of Concern
Noting more than 39 million COVID-19 cases nationwide, (as of 9/2/21) Guest projects this will continue to rise rapidly and eclipse one million a week. While “hot spots” for outbreaks clearly correspond to the country’s most lightly vaccinated locales, the impact of the delta variant is being felt in virtually every state. “There’s almost nowhere you can go in the U.S. that you don’t need to be masked indoors, even if vaccinated,” she says. The progressive increase in vaccinated patients with COVID-19 in European hospitals is also troubling, says Kinch, a potential harbinger of what is to come for the U.S.
However, what’s driving the surge is not cases among the vaccinated, known as “breakthroughs.” It’s a term Guest would like to eliminate permanently, given its negative connotation regarding vaccine efficacy. “These type of infections are still rare. More than 90% of those hospitalized with COVID-19 are unvaccinated.” She points out that while viral loads in patients with COVID-19 are the same for vaccinated and unvaccinated patients in the first few days of illness, they drop much faster and further in the vaccinated.
The vaccine, contends Kinch, was never intended to eliminate all possibility of getting COVID-19. “It’s not a suit of armor,” he says, “because no vaccine ever provides 100% protection. But we know they work incredibly well to prevent you from getting very sick or dying.”
The FDA’s recent approval of the Pfizer mRNA vaccine, with Moderna approval expected to follow soon, is pivotal, says Guest, in helping launch vaccination requirements at businesses, schools and other locations. “Don’t underestimate the importance of this approval in providing support for mandates that will protect all of us,” she says. “Recognize that in the entire history of vaccines, there has never been a set more studied than the ones we have now.”
Adds Kinch, “With the enormous amount of data gathered on the vaccines’ efficacy and safety, those who think of themselves as vaccine hesitant may more accurately be described as vaccine resistant.”
Third Doses and Boosters
The recent approval of a third dose of Pfizer or Moderna for immunosuppressed patients who didn’t build sufficient immunity from the first two doses applies to just 3% of the adult population. For everyone else (with the exception of pregnant women), a booster shot six to eight months after the initial series is being considered for approval.
“Right now, that’s how long we believe we can go without significantly diminished immunity,” says Guest. Antibody tests are not proven to be an accurate measure of protection from COVID-19, says Kinch, because the antibody levels vary by individual.
If you received Pfizer or Moderna initially, choose the same for a booster. Notes Kinch: “There’s no difference between these two vaccines—one is not better than the other.” In fact, some studies show no impact on efficacy from switching brands, he says; Johnson & Johnson data is yet to come.
And where does the flu shot fit in this fall? Absolutely essential, both agree, with the only caution that a two-week separation between the two vaccines may be recommended by some healthcare providers to avoid triggering a hyperactive immune response.
Protecting our Children
The best way to keep youngsters under 12 safe is ensuring that everyone around them is vaccinated, says Guest.
“Teachers, caregivers, babysitters and others should be vaccinated, or fully masked whenever they’re with children,” she advises. A different dose is being tested for 5- to 12-year-olds, with approval possible later this year.
The Next Wave of Variants?
While not identified by the Centers for Disease Control (CDC) as a “high concern,” Kinch admits that the lambda variant worries him primarily because not enough is known about its ability to resist vaccines. “One view is that the COVID-19 spike protein can only mutate to a certain point, and if that’s true, lambda could be the end of the virus. The other view is that we don’t know if it stopped mutating,” he says.
“We’re not defenseless, though,” counters Guest, “because we can keep it from getting here by having COVID-19 not circulating in communities. Greater numbers of vaccinated people will prevent us from getting whatever variant might follow delta.”
Stay Safe and Well
One of last year’s most popular signoff lines takes on new resonance as our experts advise on what that now means for the vaccinated in fall 2021.
Mask Up, Indoors and Out.
Masks are increasingly needed outside in crowded areas. Indoors, remember that while a soft, comfortable cloth mask protects others from you, if you need extra protection in certain settings, use a KN95 or N95 mask.
Pass on Indoor Dining, Movies, Concerts and Sporting Events.
Also reconsider full-capacity outdoor events with no masking/distancing/vaccine requirements. (As an alternative, order take-out and support virtual events offered by local venues). And avoid getting together in person with those who are not vaccinated.
Reach out to Every Unvaccinated Person you Know.
“The best action we can take is to keep encouraging every unvaccinated person we know to get the shot, now,” advises Guest. “We’re all in the race against variants and need to work together to defeat them as quickly as possible.” Adds Kinch, “It’s unfortunate that the motivations behind much of the messaging has messed up the message itself. Be completely honest about what is known and not known about the vaccine.”
The Swiss Cheese Respiratory Pandemic Defense.
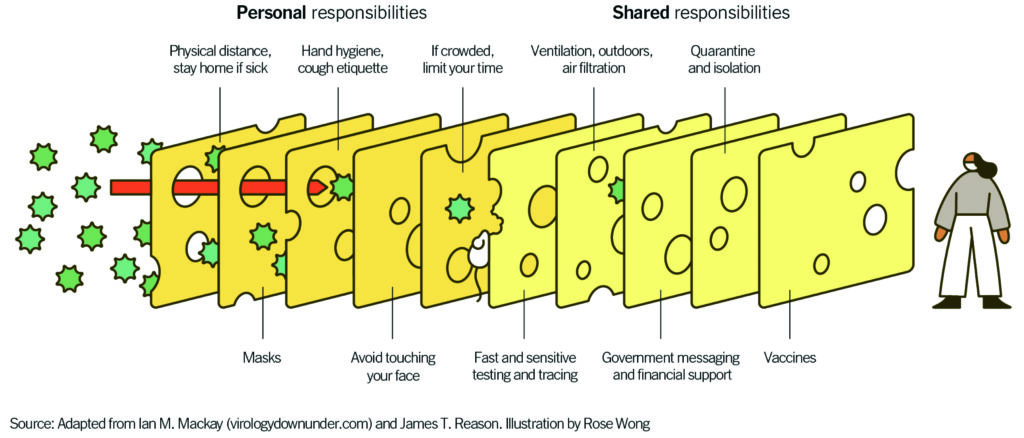 “Layering prevention messages is crucial because the delta variant has made the holes in the Swiss cheese slice of the vaccine just a bit bigger,” says Guest. “Now masks are more crucial than ever before.”
“Layering prevention messages is crucial because the delta variant has made the holes in the Swiss cheese slice of the vaccine just a bit bigger,” says Guest. “Now masks are more crucial than ever before.”
Dr. Jodie Guest is professor and vice chair of the Department of Epidemiology, Emory University, Atlanta, and award-winning leader of Emory’s Outbreak Response Team for COVID-19.
Dr. Michael Kinch is associate vice chancellor and founder/director of the Center for Research Innovation in Biotechnology and the Center for Drug Discovery at Washington University, St. Louis.
by Ivan | Oct 12, 2020 | Medical Conditions, Patient News

An Epidemiologist Separates Fact from Fiction and Offers Hope for the Future
Epidemiologists seek to learn why, how and when some people contract diseases when others don’t. Their findings are used to help monitor public health status, develop new medical treatments and disease prevention efforts, and provide an evidence base to healthcare and policy leaders.
Whether you feel the coronavirus is receding or set to surge, that testing is plentiful or inadequate, or that cases are reported as too high or too low may vary considerably based on where you live and your political leanings.
For an objective, no-spin perspective, we checked in with Jodie Guest, PhD, an epidemiologist at Emory University in Atlanta. Dr. Guest’s life’s work is studying the distribution, causes, prevention and control of diseases in populations.
Her answers to some of today’s most important questions about COVID-19 are below. Please note these reflect the situation mid-September…check our website for further updates.
Q: Are we seeing a slowdown in the number of new COVID-19 cases in the U.S.?
Dr. Guest: The number of new cases has, fortunately, plateaued or slowed down, but in many places the plateaus reflect substantially higher numbers than were reported in April, when everyone was still staying home. My concern is with schools and businesses reopening and less willingness to follow safety guidelines, the numbers may creep back up.
Q: What sites do you trust for accurate reporting on COVID-19?
Dr. Guest: I compare numbers from Johns Hopkins, Centers for Disease Control (CDC) and Worldometer to see if they match.
Q: What is the significance of the latest report from the CDC that just 6% of coronavirus deaths to date have COVID-19 as the only cause of death?
Dr. Guest: It’s not at all surprising for two reasons. One is that more than 60% of Americans have an underlying condition, such as obesity or diabetes. The risk of complications and hospitalization for people with two to three underlying conditions who contracted the virus is up to five times greater than for people with no [underlying] conditions. Second, death certificates list everything that may have contributed to mortality, including comorbid conditions and conditions caused by COVID-19 such as pneumonia. This does NOT mean that any of the more than 200,000 people who had heart disease or diabetes as an underlying condition didn’t actually die of COVID-19.
Q: Why are people of color and Latinos at greater risk of death from COVID-19?
Dr. Guest: This is not about a genetic risk of death. It’s driven by multiple factors, including a higher incidence of underlying conditions, less access to proper healthcare, greater risk of infection at the workplace and crowded living conditions that preclude social distancing.
Q: What is your take on the revised CDC guidelines that say testing for people who have been exposed to COVID-19 should be limited to those with symptoms?
Dr. Guest: Many of us in the public health community feel very strongly that we need to be testing asymptomatic people. From a public health perspective, more testing of asymptomatic people, not less, must be done to control the virus. NOTE: As of 9.18.20, CDC guidelines were revised again to state: “if you have been in close contact, such as within 6 feet of a person with documented SARS-CoV-2 infection for at least 15 minutes, and do not have symptoms, you need a test.”
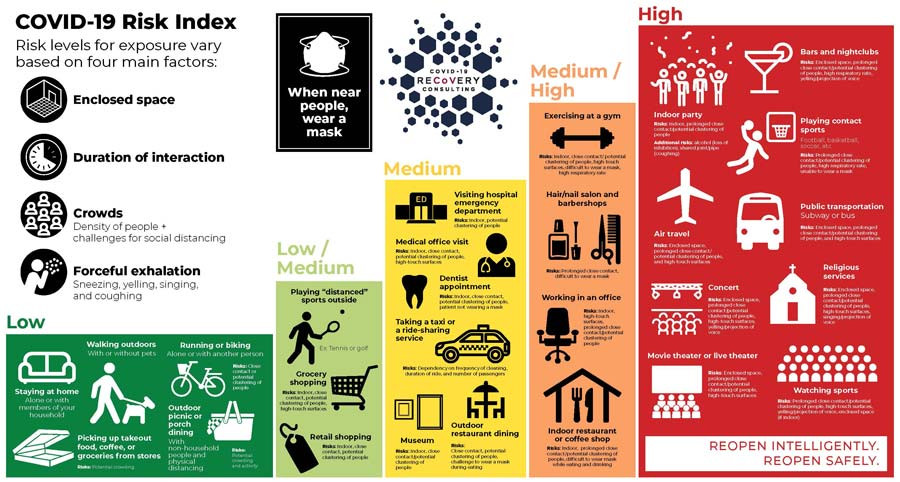
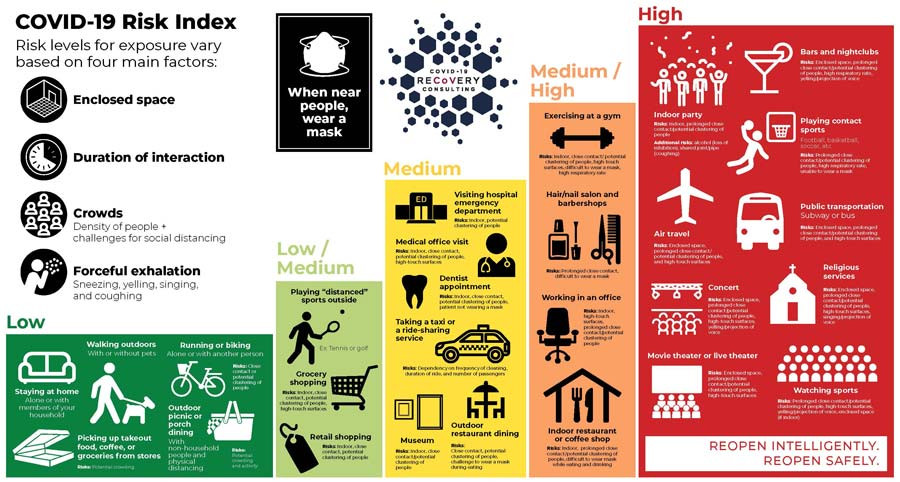
Q: What are the relative risks of activity as we move forward?
Dr. Guest: There’s so much variation based on how carefully an activity is done, but there are four good rules that apply to all: Outside is safer than inside, shorter time is safer than longer, small groups are safer than bigger, and distance is safer than closeness.
Q: How might COVID-19 affect the epidemic of flu we see annually?
Dr. Guest: If we take COVID-19 prevention measures seriously – masking, social distancing, handwashing – we could have a light flu season. If we don’t, COVID-19 will make it worse. The good news is that this has already spurred many people to get their flu shots.
Q: Any other silver linings you’re seeing?
Dr. Guest: For the first time, we are having a national conversation around health disparities and inequalities. We might actually come to a reckoning and take corrective action, and that would be spectacular.
Q: What is most important for people to know about getting back to normal?
Dr. Guest: Eventually we’ll have a vaccine but we’re not going to eliminate COVID-19 completely. However, there needn’t be this level of impact on our society. I can’t emphasize enough that we have control over how this virus spreads. We need strict guidelines and most importantly, a social contract with everyone in your community. This may be the first time many of us are asking “What are we willing to do for each other?” I hope we can all rise to the challenge.
When considering whether it is safe to resume an activity, there is much variation based on how carefully an activity is done. Additional details are provided in the infographic below, courtesy of www.covid19reopen.com
The post Can We Co-Exist with COVID-19? appeared first on Specialdocs Consultants.
by Specialdocs Consultants, LLC | Feb 1, 2020 | Medical Conditions, Patient News

Oh, My Aching Head
A dull pressure, a sharp pain, an uncomfortable pounding, a vise-like sensation – all can signal the start of a headache. A painful part of the human condition since the beginning of time, more than 150 different types of headaches have been identified, categorized and treated in increasingly effective ways. We take a look at how to cope with the most common headaches, as well as when your symptoms indicate immediate attention is needed in this great reference guide to headache types and remedies.
 Tension Headache
Tension Headache
It’s the rare person who hasn’t experienced the tight feeling or band-like grip around the head that characterizes a tension headache. Stress is frequently the trigger, so staving them off with recognized stress management strategies such as deep breathing exercises, yoga, meditation, and progressive muscle relaxation may help. For immediate relief, gentle massage and use of warmth or heat to ease tense neck and shoulder muscles often work well. Over-the-counter medicine such as aspirin, ibuprofen or acetaminophen may also be used judiciously.
Cluster Headache
Seen more often in men, these headaches cause intense pain on one side of the head or around one eye; are often accompanied by nasal discharge or teary eyes; and occur in bouts of frequent attacks over weeks or months, followed by long periods of remission. Treatments include inhaling pure oxygen through a face mask, which often relieves pain within 15 minutes, and injectable triptan medications used to treat migraines.
Exertional Headache
Headaches experienced after strenuous exercise may result from being dehydrated or overheated or simply from overexertion, and are usually resolved quickly with rest and adequate hydration.
Sinus Headache
The pain, pressure and fullness in cheeks, brow or forehead, often accompanied by stuffy nose, fatigue and an upper toothache, can indicate a headache from sinusitis or seasonal allergies, but be aware that in many cases it is actually a migraine. Rest, fluids, decongestants and over-the-counter pain medications help alleviate headaches caused by sinusitis; those caused by an allergy will usually be treated with a nasal spray.
Each headache has its own “flavor,” but if they occur more frequently or more severely, seem to worsen with the use of over-the-counter drugs, and interfere with your normal activities, please contact us…and consider starting a headache journal that you can bring to your appointment. Track if they are occurring at certain times of day, or after specific activities or foods; e.g., after a workout, a sleepless night or a change in diet. Also note the duration of each headache; where the pain is located; the intensity and type of pain; other accompanying symptoms, such as gastrointestinal distress; and medications you used. Pre-formatted trackers can be accessed online at sites such as headaches.org.
When to seek help promptly: If your headache can be described as one of the worst you’ve ever experienced and is accompanied by trouble seeing, speaking or walking; fainting; high fever; numbness, weakness or paralysis on one side of your body; stiff neck; or nausea or vomiting.
Inside the ‘Migraine Brain’
Despite the prevalence of migraine headaches, which affect 39 million people in the U.S. alone, their complex and multifactorial causes have made it difficult to pinpoint the most effective management of often debilitating symptoms that can include severe, pulsating pain; nausea; and visual auras. But years of research into the “migraine brain” are revealing a deeper understanding and new treatments, discussed in our Q&A with a headache expert, below.
Q: What is a migraine brain?
A: We have found it’s wired somewhat differently than the average brain, highly sensitive to light, sound and movement.
Q: Does genetics play a role?
A: Absolutely, as more than 70% of migraine sufferers have at least one close relative with the problem.
Q: What triggers a migraine?
A: Among the multiple factors are stress, hormonal shifts, time and travel changes, certain foods, inadequate nutrition, alcohol, and too much or too little caffeine. Anyone of these, or more likely, a combination, can trigger an episode. But the number one cause is the overuse of migraine medications, which triggers rebound headaches and starts a cycle of needing increasing quantities for relief.
Q: What medications are used to manage or prevent symptoms?
A: In addition to over-the-counter medications such as acetaminophen, a class of drugs called triptans that block pain signals in the brain have been used effectively for years. There are many other options, such as new biologic drugs to prevent or minimize the pain of migraines, including calcitonin gene-related peptide (CGRP) inhibitors and serotonin-receptor agonists.
Q: Will lifestyle adjustments make a difference?
A: There is no question that migraine patients benefit most from a set routine of healthy eating (avoiding alcohol and foods with nitrites or preservatives) and regular exercise; getting adequate sleep each night; and learning to manage stress with techniques such as biofeedback training, relaxation training and cognitive-behavioral therapy.
The post Headaches – Types and Remedies appeared first on Specialdocs Consultants.




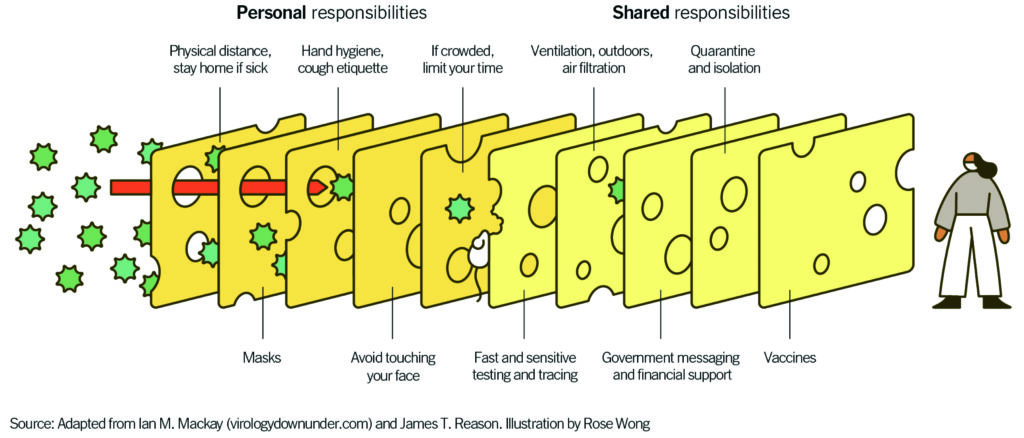 “Layering prevention messages is crucial because the delta variant has made the holes in the Swiss cheese slice of the vaccine just a bit bigger,” says Guest. “Now masks are more crucial than ever before.”
“Layering prevention messages is crucial because the delta variant has made the holes in the Swiss cheese slice of the vaccine just a bit bigger,” says Guest. “Now masks are more crucial than ever before.”

Recent Comments