
by Specialdocs Consultants | Feb 25, 2025 | Healthy Aging, Patient News
Alcohol and Cancer Risk
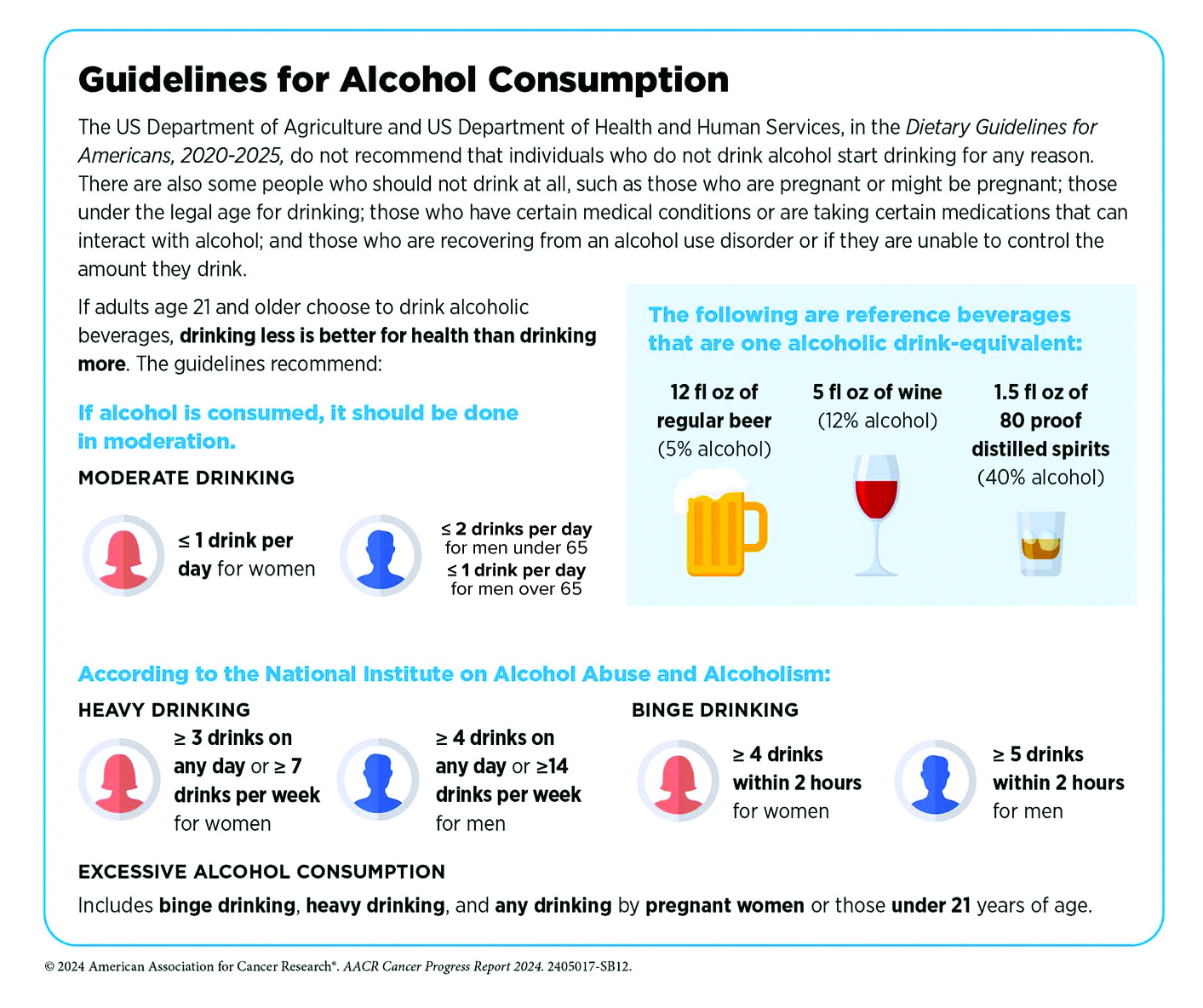
Our year was off to a sobering start with the advisory on alcohol and cancer risk issued by the Surgeon General in January. The key points, which were concerning, and for at least half of Americans, seemingly unknown until now, included:
- A direct link was reported between alcohol consumption and higher risk for cancers of the breast, colorectum, esophagus, liver, mouth, throat (pharynx), and voice box (larynx).
- Four pathways were posited: 1) As it metabolizes, alcohol breaks down into acetaldehyde, a chemical which damages DNA in multiple ways. This can cause a cell to begin growing uncontrollably and create a cancerous tumor. 2) Alcohol induces oxidative stress, damaging DNA, proteins, and cells, and increasing inflammation. 3) Alcohol may alter hormone levels, which can play a role in development of breast cancer. 4) Carcinogens from other sources, especially particles of tobacco smoke, can dissolve in alcohol, making it easier to be absorbed into the body, and increasing risk for mouth and throat cancers.
- Citing a 2019 survey showing that just 45% of Americans recognize alcohol as a risk factor for cancer, a strong recommendation was made to raise awareness by updating the current warning label on alcoholic beverages.
There is no doubt that the Surgeon General can greatly influence recognition of a health issue, as evidenced by the landmark 1964 report on the risks of tobacco, laying the groundwork for public regulations in the decades to follow. Then, 42% of Americans smoked, now just 11% do. The impact of the current alcohol advisory may not be as profound, but it is significant for several reasons.
While the science behind the advisory is not new, as alcohol-related cancer risk has been noted previously by many healthcare organizations, it has grown increasingly stronger over the years. Particularly for women who drink, recent studies have added to the mounting evidence of their higher risk of developing breast cancer, as well as increased susceptibility to liver disease, cardiovascular disease, and neurotoxicity compared to males. A more widespread public campaign with prominent warnings on alcohol-containing products will help underscore these findings.
The advisory may also add impetus to the cultural shift around alcohol use that’s been occurring over the last decade. As noted, the percentage of Americans who agreed that 1-2 drinks per day is bad for one’s health is low at 45% in the most recent Gallup poll but still reflects a marked improvement compared to 26% in 2016. Most promisingly, the younger generation is leading the charge, with 65% of adults aged 18 to 34 agreeing that alcohol consumption negatively affects health vs. 38% on average of their elders.
Highlighting the risk of disease associated with alcohol requires a more nuanced approach than tobacco, where no consumption is considered safe. Instead, alcohol consumption is viewed along a continuum where risk for most people remains relatively low at 2 standard drinks or less per week, and moderately low at 3 to 6 standard drinks per week – yet fully acknowledging that individual risk is determined by a complex interaction of biological and environmental factors. As long-time researchers wrote in the Harvard Public Health Journal, while heavy drinking is indisputably harmful at every age, the data may not justify sweeping statements about the effects of moderate alcohol consumption. They point to research with mixed results e.g. studies showing decreased mortality, lower risk of cardiovascular disease in moderate drinkers, and a widely cited UK study of one million women that reported higher rates of breast cancer among drinkers but lower rates of thyroid cancer, non-Hodgkin lymphoma, and renal cell carcinoma. Recognizing that a gold-standard randomized control study would be well-nigh impossible to conduct, the most reasonable approach is to equip people with information that allows them to understand why less alcohol is better, and zero risk is only possible at zero consumption.
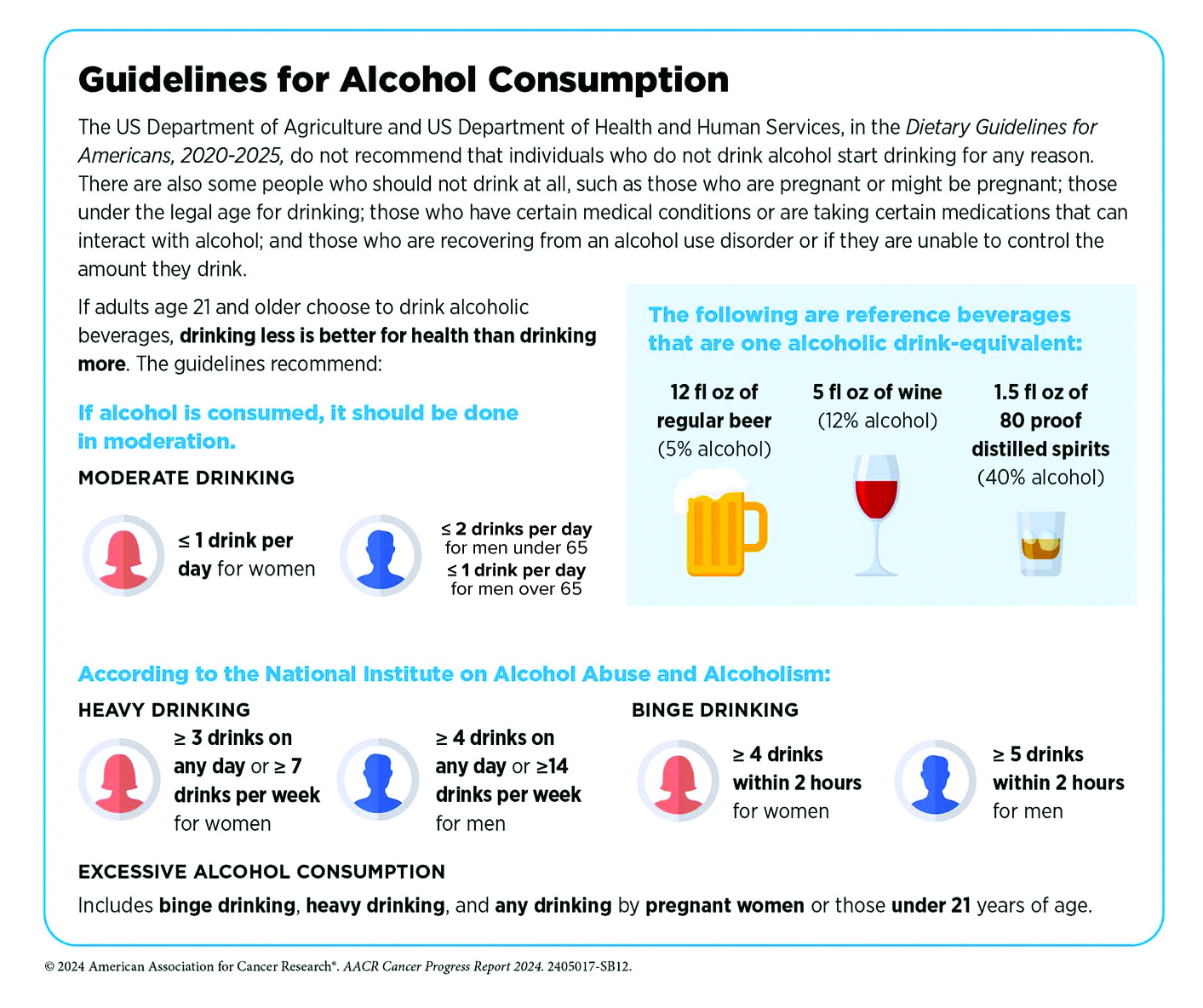
Our recommendations:
If you don’t drink, don’t start, as benefits are unproven, and the downsides are clear. Avoid alcohol completely if you are pregnant or trying, have a personal or family history of alcohol use disorder (AUD), have a medical condition that alcohol can aggravate (e.g., liver disease, precancerous conditions of the digestive tract), use medication that can cause interactions, or operate potentially dangerous machinery. However, if you are debating whether you can enjoy an occasional glass of chardonnay, please talk to us. We’ll help you make an informed decision based on multiple factors, including age, gender, medical history, diet, fitness, and lifestyle.
Symptoms of Alcohol Use Disorder (AUD)
What defines a heavy drinker, or a person with AUD? If you’ve experienced two or more of these symptoms in the past year, you may benefit from professional guidance to help you decrease or stop alcohol consumption:
- Had times when you ended up drinking more, or longer, than you intended?
- More than once wanted to cut down or stop drinking, or tried to, but couldn’t?
- Spent a lot of time being sick from drinking, or getting over other aftereffects?
- Wanted a drink so badly you couldn’t think of anything else?
- Found that drinking—or being sick from drinking—often interfered with taking care of your home or family, or caused job troubles?
- Continued to drink even though it was causing trouble with your family or friends?
- Given up or cut back on activities important to you to drink?
- Gotten into unsafe situations while or after drinking e.g., driving, walking in a dangerous area?
- Continued to drink even though it was making you feel depressed/anxious or after an alcohol-related memory blackout?
- Found that your usual number of drinks had much less effect than before?
- Experienced withdrawal symptoms when the effects of alcohol were wearing off e.g., trouble sleeping, shakiness, restlessness, nausea, sweating?
Sources: Harvard Public Health, Journal of Internal Medicine, Journal of the National Cancer Institute, Surgeon General’s Advisory on Alcohol and Cancer Risk, UptoDate, Rethinking Drinking, National Institutes of Health
by Specialdocs Consultants | Feb 24, 2025 | Healthy Aging, Patient News
Whether you’re a healthy 40-something with a family history of premature cardiac events, a 50-year-old mother who experienced a complicated pregnancy decades ago, or a 65-year-old man whose statin treatment has failed to lower high cholesterol levels, take heart in the growing arsenal of tests and therapies aimed at preventing disease. A long-time advocate for proactive, preventive cardiac care, Dara Lee Lewis, MD, a cardiologist at Boston’s Lown Cardiology Group and Assistant Professor at Harvard Medical School, shares insightful updates in the Q&A below.
Q: What do you see as some of the most promising recent developments in preventive heart care?
A: As a cardiologist, I’m trained to help patients live well with chronic conditions like coronary atherosclerosis, heart failure and atrial fibrillation. But let’s face it – by the time patients are referred to me, their cardiac disease is already established. Wouldn’t it be better to prevent these diseases from developing in the first place? While we can do an excellent job minimizing symptoms and stabilizing disease, I’m just treating the tip of the iceberg. We know that atherosclerosis, or hardening of the arteries, takes decades to develop. The time for intervention is in the iceberg itself, before that first heart attack, when someone may feel fine but under the surface, disease is brewing. That’s where risk factors such as inflammation, pre-diabetes, high cholesterol levels, and unhealthy behaviors are putting the patient at risk. We have the opportunity to make a huge impact by working with our primary care colleagues to identify high-risk patients at the earliest stages and reduce the chance of having a cardiovascular event in the first place.
Q: In addition to the well-documented factors that can signal a person at high risk for heart disease – unhealthy cholesterol levels, hypertension, diabetes, metabolic syndrome, smoking, lack of physical activity, age, family history – have others been identified?
A: Yes, we’re beginning to better understand the key role inflammation plays in the development of coronary artery disease, and now consider chronic inflammatory conditions such as gingivitis, rheumatoid arthritis and certain autoimmune disorders to be risk factors. Women who experienced a complicated pregnancy history, premature menopause or certain cancer treatments are also at a higher risk of heart disease and require close monitoring and screening throughout their lifetime. Most notably, elevated levels of lipoprotein (a), known as Lp(a) (a subtype of LDL cholesterol), have been identified as an independent risk factor.
Q: Why is Lp(a) so significant?
A: An elevated Lp(a), greater than 30-50 mg/dl, is often present in otherwise healthy people. It is a genetically determined risk factor for heart disease, peripheral artery disease, and ischemic stroke. What makes this challenging is that traditional strategies for lowering cholesterol such as statins or exercise and diet modifications have little to no effect on Lp(a); however, PCSK9 inhibitors (non-statin therapy for lowering cholesterol), hormone replacement therapy and Tamoxifen can work for certain individuals. There are also some promising newer medications currently being studied.
Q: Sometimes statins (e.g. Lipitor, Crestor) don’t work to lower LDL or ‘bad’ cholesterol either…are other options available?
A: A number of non-statin therapies can be prescribed, including:
- Ezetimibe (Zetia), a relatively inexpensive pill that can be used alone or given with statins to reduce cholesterol absorption.
- PCSK9 inhibitors (e.g. Praluent, Repatha), monoclonal antibodies given as a shot every two to four weeks. These inactivate the protein PCSK9 to promote more LDL receptors and help clear LDL from the bloodstream.
- Bempedoic acid (Nexletol), a daily pill that causes the liver to make less cholesterol, but with fewer of the muscle aches experienced by some who take statins.
- Inclirisan (Leqvio), given as a shot twice yearly, blocks production of PCSK9.
- Evinacumab (Evkeeza), a monthly infusion approved only for people with a family history of hypercholesterolemia.
Q: Are there any new tools for calculating an individual’s risk of heart disease?
A: I’ve found the American Heart Association’s new PREVENT calculator to be a convenient resource to assess an individual’s risk of heart attack, stroke or heart failure over the next 10 and 30 years. It’s more comprehensive than earlier versions, as it includes measures of kidney function and metabolic health and can be used to predict risk in patients as young as age 30, which is extremely valuable in terms of early detection.
by Specialdocs Consultants | Feb 24, 2025 | Patient News
“A lie can travel halfway around the world while the truth is still putting its boots on.” *
It’s not easy to cut through the clutter in our world of often viral misinformation and find irrefutable facts. Healthcare is especially prone to misinterpretation because the scientific method—developing, testing, experimenting and refining hypotheses—can seem imperfect but is fundamental to reaching a solid conclusion. As the evidence evolves, previous findings may be corroborated, but may also be contradicted. Importantly, even some widely publicized studies may be unreliable or not based on a solid foundation. All of which proves frustrating to people seeking unequivocal advice on issues ranging from nutrition (is a low fat diet healthier than a high protein one?) to exercise (are 10,000 daily steps necessary or will 5,000 do?) to longevity (can a healthy lifestyle overcome challenging genetics?). No definitive answers just yet, but as new research reports continue to flow in, we offer this short guide to help you identify the characteristics of a good, credible scientific study.
- Randomized design, where participants are divided into control and test groups in a random manner to minimize the chance of bias. This is the gold standard of research, ensuring findings are causal and not confounded by other factors.
- Double-blinded, where neither participants or researchers are aware of whether the participant is in the control or test group.
- Observational, where the effects of a risk factor or treatment are studied over time without changing who is or isn’t exposed to them; used to develop the Surgeon General’s advisory on alcohol and cancer risk.
- A large enough sample size to have statistically significant findings, and allow for a range of individual differences.
- Has been replicated by other researchers.
- Results published in a peer-reviewed, respected professional journal, with no conflicts of interest reported by the researchers.
*Has been erroneously attributed to Mark Twain; but actually appeared in the 1859 book Spurgeon’s Gems by Rev. CH Spurgeon.
Set Your Sites
Start with any of these 18 websites for trustworthy health information:
-
- Mayoclinic.org – Mayo Clinic guide to diseases and conditions
- HopkinsMedicine.org – Johns Hopkins Medicine
- Health.Harvard.edu – Harvard Health Publishing – Harvard Medical School
- MerckManuals.com – Consumer version of medical reference book used by physicians since 1899
- EatRight.org – American Academy of Nutrition & Dietetics
- Heart.org — American Heart Association
- Diabetes.org — American Diabetes Association
- FamilyDoctor.org – American Academy of Family Physicians
- HealthChildren.org – American Academy of Pediatrics
- Sexetc.org – Teen sexual health information, sponsored by Rutgers University
- Meopause.org – National Menopause Society
- HealthinAging.org – American Geriatrics Society
- TheConversationProject.org – Advanced care planning
- NCCN.org – National Comprehensive Cancer Network
- NAMI.org – National Alliance on Mental Illness (NAMI)
- Rarediseases.org – National Organization for Rare Diseases
- VeryWellFit.com – Very Well Fit
- ACEFitness.org – American Council on Exercise

by Specialdocs Consultants | Nov 21, 2024 | Nutrition, Patient News
As dietary restrictions become more commonplace (an estimated 10% of Americans have a food allergy, another 5% are vegetarian or vegan), serving a holiday meal that satisfies a diversity of diners may seem intimidating. Below we show some easy ways to deconstruct or reconstruct your dishes to give everyone – whether they’re heart-healthy, diabetic, gluten-sensitive, lactose-intolerant, nut-free or plant-forward – a prime seat at the table.
Keep it fresh
Opt for meats or poultry that haven’t been pre-seasoned or injected with a brine that adds sodium and sugar. Offer a small tofurky as an alternative option for committed vegetarians and adventurous eaters.
Keep it traditional with a twist
Prepare a rice-based stuffing or quinoa-centric pilaf with time-honored holiday seasonings like celery, sage and thyme. Swap out canned cranberry sauce, high in preservatives and sugar, for a tasty new recipe of fresh cranberries boiled and simmered with fruit juice, applesauce and orange zest.
Keep it versatile
Small adjustments can make a big difference. Use olive oil instead of butter, vegetable stock instead of chicken or beef broth, or a plant-based milk instead of regular.
Keep it neutral
Serve sauces and gravies on the side so everyone can enjoy the main dish without concerns about hidden allergenic ingredients.
Keep it simple
Place nuts, croutons, cheese, dried fruits and dressings adjacent to the greens, and let guests build a salad according to their individual preferences.
Keep it seasonal
Pile a colorful selection of winter’s best, from sweet potatoes and beets to broccoli and Brussels sprouts, in a single layer on a baking sheet, spray lightly with olive oil, season with black pepper and herbs, and roast at 425 degrees for about 45 minutes. The heat will coax out the exquisite natural flavors in the veggies for a dish that’s suited to any type of diet.
Keep it light
Substitute apple sauce for oil when baking to cut down on fat and sugar.
Keep it non-alcoholic
Stir up an appealing selection of ‘mocktails’ for all who choose not to imbibe.
Allergens: Off the Plate
Be aware of these ingredients, which account for more than 90% of all food allergies:

- Fish
- Milk
- Peanuts
- Crustacean shellfish
- Soybeans
- Tree nuts
- Wheat
- Eggs
- Sesame (added in 2021)
Sources:

by Specialdocs Consultants | Nov 20, 2024 | Mental Health, Patient News
If your parents repeatedly exhorted you to count your blessings, it may well prove to be one of the best pieces of medical advice they shared. In this season of giving and thankfulness, we share a brief synopsis of how gratitude – defined as appreciation of what is valuable and meaningful to oneself – is associated with a host of beneficial health effects.
Mental Health
A grateful outlook may contribute to lower rates of depression, stress and anxiety, greater emotional functioning, stronger social relationships, higher life satisfaction, and help reduce the impact of stress on negative health outcomes.
Physical Health
Studies suggest that an attitude of gratitude may help lower blood pressure and glucose, improve immune function, promote more efficient sleep, boost pain tolerance, and lead to better cardiovascular health. Specifically, research has pointed to how practicing gratitude may help decrease hemoglobin A1c levels and contribute to reducing biomarkers of inflammation. A recent observational Harvard study of more than 49,000 registered nurses found that those scoring in the highest level of gratitude had a 15% lower risk of death from cardiovascular disease. Other reports have found that grateful individuals tend to be more health-conscious, avoiding smoking and drinking alcohol. For instance, a recent experimental study showed that evoking feelings of gratitude in people who smoke reduced their urge to do so and increased the likelihood of their enrollment in smoking cessation programs.
The Gratitude and Health Connection
Taken together, research suggests that interventions targeted at increasing gratitude may be an effective resource for health promotion and maintenance. Or as Dr. Robert Emmons, a long-time leader in the field of gratitude research and professor emeritus of psychology at UC-Davis, more eloquently explains:
“Gratitude heals, energizes and changes lives. Studies have shown that gratitude is often deepened and strengthened in trying times, as they lead us to not take things for granted. Gratitude is not simply a switch that we turn on when life is going well, but also shines a light in the darkness.”
Interested in trying this out? Visit UC Berkley’s Thnx4.org site, which offers free 10- or 21-day group or solo journaling challenges.

by Specialdocs Consultants | Nov 20, 2024 | Nutrition, Patient News
In the past decade it has become well recognized that the millions of bacteria in the gut, collectively known as the microbiome, can influence the health of the brain, lung, heart, metabolism and the immune system. Thousands of studies have been conducted since the term was first introduced in 2001, with research shifting from an early focus on cataloging microorganisms in the human microbiome to pathogen identification and now to understanding their functional roles and how they interact with the host. Following are some of the key learnings to date, including a conversation with a leading microbiome researcher on behalf of our Well Read Patient readers. Please keep in mind that microbiome research is still in its infancy, and probiotic/prebiotic treatments are not the standard of care at this time.
What exactly is the microbiome?
Scientists define it as the sum of the microorganisms (bacteria, viruses, fungi, etc. that live in the body in healthy conditions), their genetic information, and their ecological niches. The microbiome is spread across different organs and tissues of the human body, but the most important and best studied is the gut microbiome. Studies show that under normal conditions, formation of the adult gut microbiome occurs over the first 3 years of life and is affected by events such as birth method, cessation of breastfeeding and starting solid food. Over time, it is thought that diet, drugs, age, smoking, exercise and host genetics affect the composition of the gut microbiome, and that some of these changes may contribute to metabolic, neurological, and immune disorders.
A high fiber, low animal fat diet may have beneficial effects on the gut microbiome. With this in mind, the principle of “You are what you eat” is further clarified as “You are what your gut microbes do with what you eat,” according to the European Society of Neurogastroenterology & Motility. This is precisely the area that has long fascinated Christopher Damman, MD, a gastroenterologist who has studied the microbiome’s role in health and disease for the past two decades.
“While there are many ways to consider the role microbes play in our health, most essentially they activate or transform components of food that the body can’t process by itself,” he explains. “The microbiome converts polyphenol, the colorful compounds that occur naturally in plants, and fiber, a carbohydrate prebiotic that resists host digestion, to metabolites, which are molecular byproducts of digestion. These in turn influence the mitochondria, our cells’ metabolic powerhouses, that generate most of the energy needed for the cell to function.”
Metabolites also underly the gut’s natural production of hormones GLP and GLP-1, best known for its use in weight loss and type 2 diabetes drugs like Wegovy and Ozempic. Together, with another lower gut hormone called PYY, they help coordinate the body’s response to food by regulating appetite and blood sugar.
The traditional focus has been on therapeutic use of live microbes to repopulate the gut; for some, however, says Dr. Damman, there may be more power in postbiotics. “It can be very difficult to repopulate the microbiome of individuals whose guts may resemble a bleached coral reef as opposed to a vibrant aquarium, by just increasing intake of prebiotics through whole foods. The next best approach may be to therapeutically provide the metabolites naturally produced by a healthy gut microbiome,” he says.
While the gut responds to everything in your environment, from exercise to stress levels, food appears to be disproportionately important, asserts Dr. Damman. “The key to fostering a healthy microbiome may focus on four nutrients: fiber, phenols, bioactive fats, and ferments.” To that end, he has created a tool to help guide people to microbiome-friendly choices by assigning a Nutrient Consume Score (NCS) from one to 100 for a wide range of foods. Based on an algorithm that promotes increased fiber, phytonutrients, bioactive fats and potassium, and decreased amounts of simple carbs, additives, saturated fats and sodium, NCS is available as a prototype online at Dr. Damman’s website gutbites.org. An app is in development that will enable easier use, such as scanning UPC codes at the grocery store. “I believe this is the first microbiome-focused nutrient calculator, and my intent is to have it validated scientifically and clinically before a beta release, possibly by early next year,” he says.
The takeaway from all this is deceptively simple. “We have gone on these really interesting, complex journeys intellectually, but at the end of the day, we return to our original understanding of healthy eating,” muses Dr. Damman. “As Michael Pollan (influential best-selling author and fellow at the Radcliffe Institute for Advanced Study at Harvard) says, eating mostly plant-based food, and not too much, is the way to go. All the research on the microbiome, metabolites, mitochondria, bioactives, etc. points in screaming ways right back at something we’ve known all along. We’ve evolved over centuries in concert with our microbiome and healthy whole foods that naturally regulate our appetites.”
In terms of preventing obesity, diabetes and metabolic disease, Dr. Damman maintains: “There’s no substitute for a healthy diet complemented by mindfulness, movement, and adequate sleep.”
New Tools, New Strategies for Gut Microbioma Therapy

Initially, gut microbiome therapies ranged from probiotics and prebiotics to fermented foods and fecal transplants.
But these are still early days, and new approaches are continually under the microscope, including:
- According to research from Nature Aging, in healthy individuals the microbiome can continue to change after age 50, in contrast with a static microbiome composition seen in people who are less healthy and die earlier. Of particular note is the finding that each person’s microbiome becomes more distinct as they age, emphasizing the ineffectiveness of a ‘one size fits all’ approach and influencing the need for personalized health therapies.
- Mayo Clinic’s recently announced Gut Microbiome Wellness Index 2, a tool designed for healthcare practitioners to identify adverse changes in their patients’ gut health before serious symptoms arise. By screening a gut microbiome sample, the tool can predict with 80% accuracy or greater whether a person’s gut is healthy or trending toward a diseased state. The ability to detect shifts in gut health was tested in various clinical scenarios, including people who had undergone fecal microbiota transplantation, or had made changes in dietary fiber intake, or who had antibiotic exposure. Additional testing is in progress.
- New technologies that allow physicians to more easily examine the small intestine and upper part of the colon are sure to shine a bright light on these often neglected areas of microbiome research, according to Dr. Damman. Most exciting is the recent launch of swallowable devices with compartments that open up when certain acidity levels are reached to sample the small intestine. “This could be a real breakthrough for exploring how to best help those with small intestinal bacterial overgrowth (SIBO), Crohn’s, irritable bowel syndrome (IBS) and other conditions who frequently experience significant gastrointestinal symptoms from macro nutrient-rich diets.” Future possibilities may include partnering small intestine bacteria with their preferred prebiotics and personalized combinations of prebiotics.
Sources:







Recent Comments