
by Specialdocs Consultants | Feb 25, 2025 | Healthy Aging, Patient News
Alcohol and Cancer Risk
Our year was off to a sobering start with the advisory on alcohol and cancer risk issued by the Surgeon General in January. The key points, which were concerning, and for at least half of Americans, seemingly unknown until now, included:
- A direct link was reported between alcohol consumption and higher risk for cancers of the breast, colorectum, esophagus, liver, mouth, throat (pharynx), and voice box (larynx).
- Four pathways were posited: 1) As it metabolizes, alcohol breaks down into acetaldehyde, a chemical which damages DNA in multiple ways. This can cause a cell to begin growing uncontrollably and create a cancerous tumor. 2) Alcohol induces oxidative stress, damaging DNA, proteins, and cells, and increasing inflammation. 3) Alcohol may alter hormone levels, which can play a role in development of breast cancer. 4) Carcinogens from other sources, especially particles of tobacco smoke, can dissolve in alcohol, making it easier to be absorbed into the body, and increasing risk for mouth and throat cancers.
- Citing a 2019 survey showing that just 45% of Americans recognize alcohol as a risk factor for cancer, a strong recommendation was made to raise awareness by updating the current warning label on alcoholic beverages.
There is no doubt that the Surgeon General can greatly influence recognition of a health issue, as evidenced by the landmark 1964 report on the risks of tobacco, laying the groundwork for public regulations in the decades to follow. Then, 42% of Americans smoked, now just 11% do. The impact of the current alcohol advisory may not be as profound, but it is significant for several reasons.
While the science behind the advisory is not new, as alcohol-related cancer risk has been noted previously by many healthcare organizations, it has grown increasingly stronger over the years. Particularly for women who drink, recent studies have added to the mounting evidence of their higher risk of developing breast cancer, as well as increased susceptibility to liver disease, cardiovascular disease, and neurotoxicity compared to males. A more widespread public campaign with prominent warnings on alcohol-containing products will help underscore these findings.
The advisory may also add impetus to the cultural shift around alcohol use that’s been occurring over the last decade. As noted, the percentage of Americans who agreed that 1-2 drinks per day is bad for one’s health is low at 45% in the most recent Gallup poll but still reflects a marked improvement compared to 26% in 2016. Most promisingly, the younger generation is leading the charge, with 65% of adults aged 18 to 34 agreeing that alcohol consumption negatively affects health vs. 38% on average of their elders.
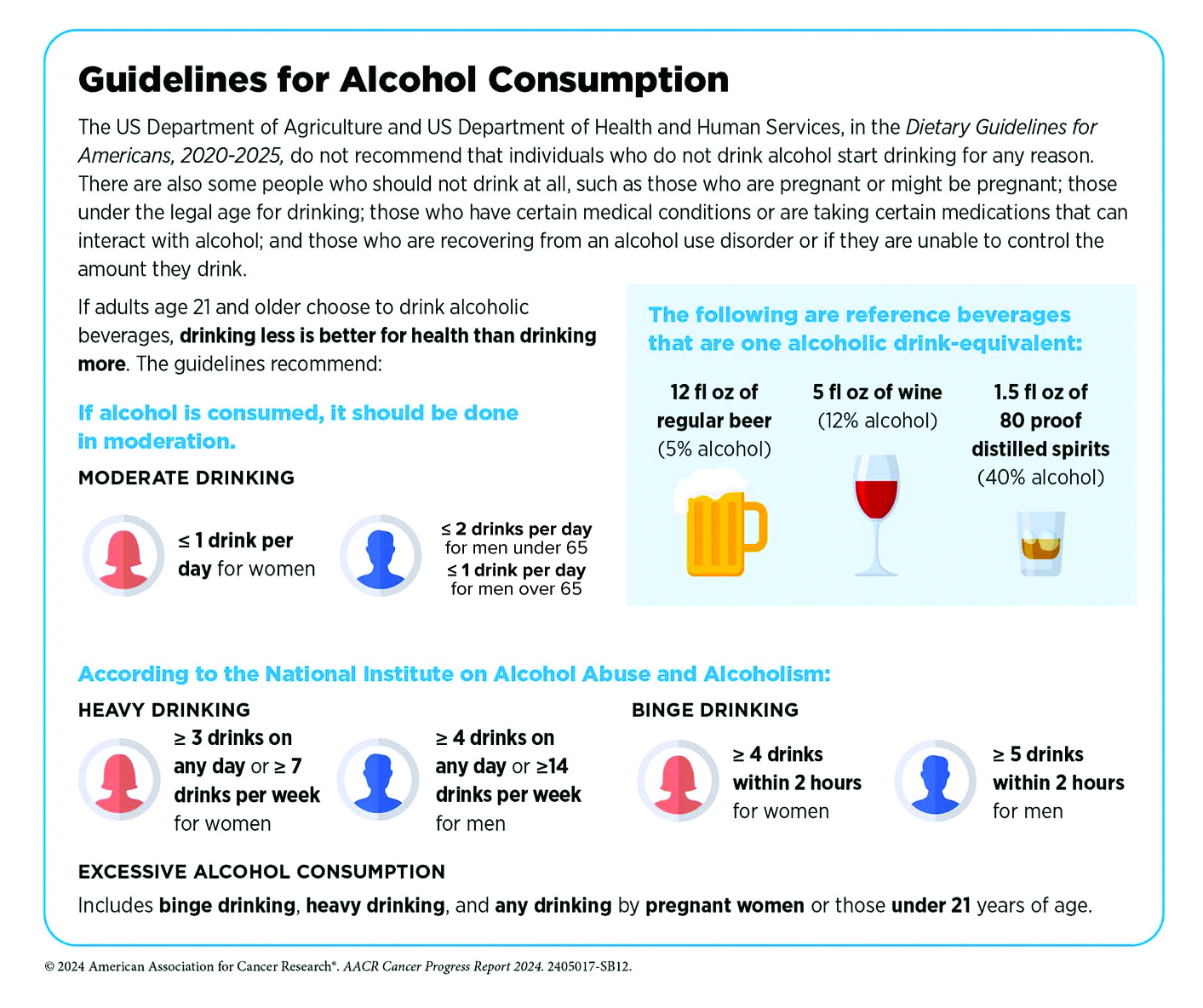
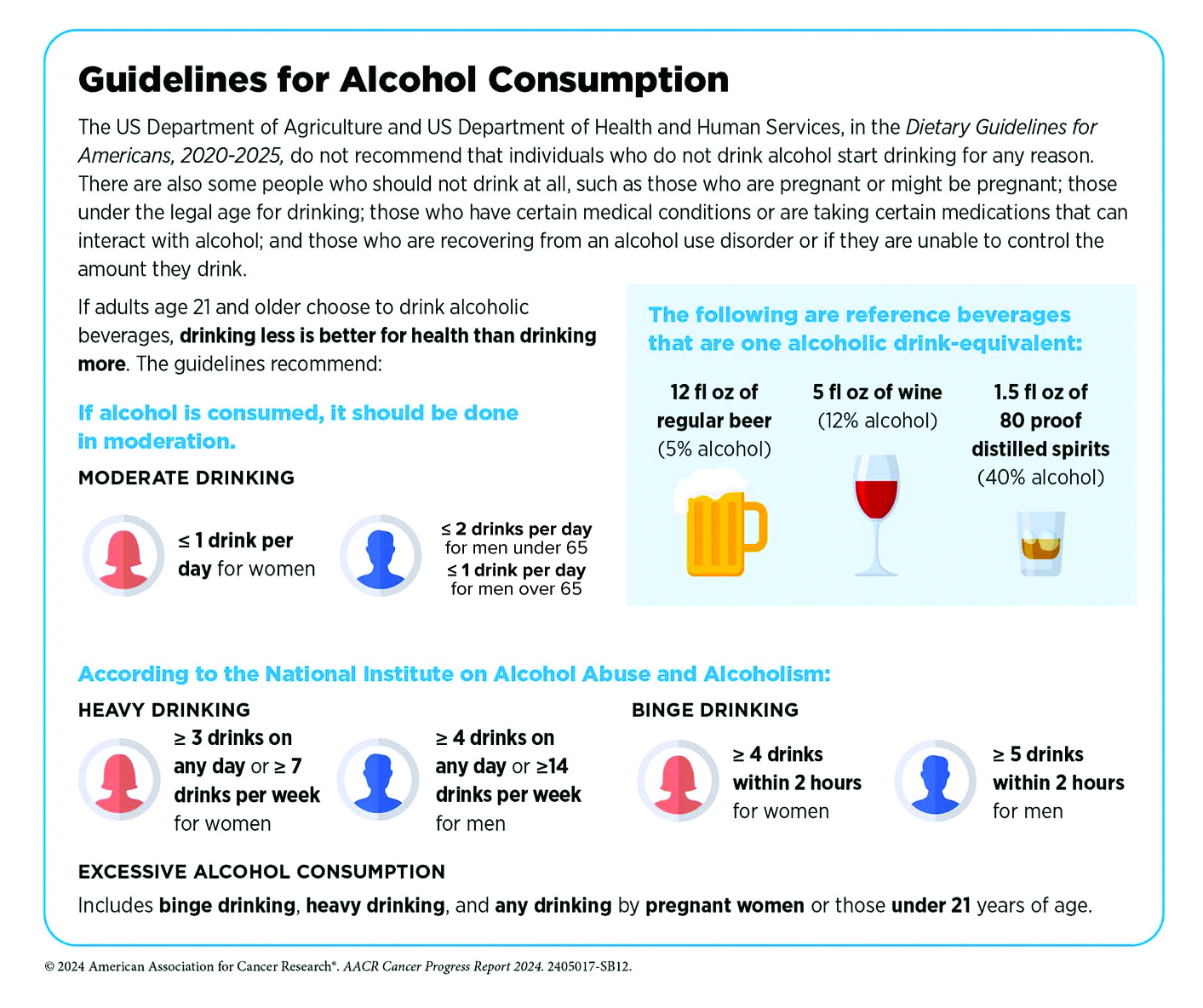
Highlighting the risk of disease associated with alcohol requires a more nuanced approach than tobacco, where no consumption is considered safe. Instead, alcohol consumption is viewed along a continuum where risk for most people remains relatively low at 2 standard drinks or less per week, and moderately low at 3 to 6 standard drinks per week – yet fully acknowledging that individual risk is determined by a complex interaction of biological and environmental factors. As long-time researchers wrote in the Harvard Public Health Journal, while heavy drinking is indisputably harmful at every age, the data may not justify sweeping statements about the effects of moderate alcohol consumption. They point to research with mixed results e.g. studies showing decreased mortality, lower risk of cardiovascular disease in moderate drinkers, and a widely cited UK study of one million women that reported higher rates of breast cancer among drinkers but lower rates of thyroid cancer, non-Hodgkin lymphoma, and renal cell carcinoma. Recognizing that a gold-standard randomized control study would be well-nigh impossible to conduct, the most reasonable approach is to equip people with information that allows them to understand why less alcohol is better, and zero risk is only possible at zero consumption.
Our recommendations:
If you don’t drink, don’t start, as benefits are unproven, and the downsides are clear. Avoid alcohol completely if you are pregnant or trying, have a personal or family history of alcohol use disorder (AUD), have a medical condition that alcohol can aggravate (e.g., liver disease, precancerous conditions of the digestive tract), use medication that can cause interactions, or operate potentially dangerous machinery. However, if you are debating whether you can enjoy an occasional glass of chardonnay, please talk to us. We’ll help you make an informed decision based on multiple factors, including age, gender, medical history, diet, fitness, and lifestyle.
Symptoms of Alcohol Use Disorder (AUD)
What defines a heavy drinker, or a person with AUD? If you’ve experienced two or more of these symptoms in the past year, you may benefit from professional guidance to help you decrease or stop alcohol consumption:
- Had times when you ended up drinking more, or longer, than you intended?
- More than once wanted to cut down or stop drinking, or tried to, but couldn’t?
- Spent a lot of time being sick from drinking, or getting over other aftereffects?
- Wanted a drink so badly you couldn’t think of anything else?
- Found that drinking—or being sick from drinking—often interfered with taking care of your home or family, or caused job troubles?
- Continued to drink even though it was causing trouble with your family or friends?
- Given up or cut back on activities important to you to drink?
- Gotten into unsafe situations while or after drinking e.g., driving, walking in a dangerous area?
- Continued to drink even though it was making you feel depressed/anxious or after an alcohol-related memory blackout?
- Found that your usual number of drinks had much less effect than before?
- Experienced withdrawal symptoms when the effects of alcohol were wearing off e.g., trouble sleeping, shakiness, restlessness, nausea, sweating?
Sources: Harvard Public Health, Journal of Internal Medicine, Journal of the National Cancer Institute, Surgeon General’s Advisory on Alcohol and Cancer Risk, UptoDate, Rethinking Drinking, National Institutes of Health
by Specialdocs Consultants | Feb 24, 2025 | Healthy Aging, Patient News
Whether you’re a healthy 40-something with a family history of premature cardiac events, a 50-year-old mother who experienced a complicated pregnancy decades ago, or a 65-year-old man whose statin treatment has failed to lower high cholesterol levels, take heart in the growing arsenal of tests and therapies aimed at preventing disease. A long-time advocate for proactive, preventive cardiac care, Dara Lee Lewis, MD, a cardiologist at Boston’s Lown Cardiology Group and Assistant Professor at Harvard Medical School, shares insightful updates in the Q&A below.
Q: What do you see as some of the most promising recent developments in preventive heart care?
A: As a cardiologist, I’m trained to help patients live well with chronic conditions like coronary atherosclerosis, heart failure and atrial fibrillation. But let’s face it – by the time patients are referred to me, their cardiac disease is already established. Wouldn’t it be better to prevent these diseases from developing in the first place? While we can do an excellent job minimizing symptoms and stabilizing disease, I’m just treating the tip of the iceberg. We know that atherosclerosis, or hardening of the arteries, takes decades to develop. The time for intervention is in the iceberg itself, before that first heart attack, when someone may feel fine but under the surface, disease is brewing. That’s where risk factors such as inflammation, pre-diabetes, high cholesterol levels, and unhealthy behaviors are putting the patient at risk. We have the opportunity to make a huge impact by working with our primary care colleagues to identify high-risk patients at the earliest stages and reduce the chance of having a cardiovascular event in the first place.
Q: In addition to the well-documented factors that can signal a person at high risk for heart disease – unhealthy cholesterol levels, hypertension, diabetes, metabolic syndrome, smoking, lack of physical activity, age, family history – have others been identified?
A: Yes, we’re beginning to better understand the key role inflammation plays in the development of coronary artery disease, and now consider chronic inflammatory conditions such as gingivitis, rheumatoid arthritis and certain autoimmune disorders to be risk factors. Women who experienced a complicated pregnancy history, premature menopause or certain cancer treatments are also at a higher risk of heart disease and require close monitoring and screening throughout their lifetime. Most notably, elevated levels of lipoprotein (a), known as Lp(a) (a subtype of LDL cholesterol), have been identified as an independent risk factor.
Q: Why is Lp(a) so significant?
A: An elevated Lp(a), greater than 30-50 mg/dl, is often present in otherwise healthy people. It is a genetically determined risk factor for heart disease, peripheral artery disease, and ischemic stroke. What makes this challenging is that traditional strategies for lowering cholesterol such as statins or exercise and diet modifications have little to no effect on Lp(a); however, PCSK9 inhibitors (non-statin therapy for lowering cholesterol), hormone replacement therapy and Tamoxifen can work for certain individuals. There are also some promising newer medications currently being studied.
Q: Sometimes statins (e.g. Lipitor, Crestor) don’t work to lower LDL or ‘bad’ cholesterol either…are other options available?
A: A number of non-statin therapies can be prescribed, including:
- Ezetimibe (Zetia), a relatively inexpensive pill that can be used alone or given with statins to reduce cholesterol absorption.
- PCSK9 inhibitors (e.g. Praluent, Repatha), monoclonal antibodies given as a shot every two to four weeks. These inactivate the protein PCSK9 to promote more LDL receptors and help clear LDL from the bloodstream.
- Bempedoic acid (Nexletol), a daily pill that causes the liver to make less cholesterol, but with fewer of the muscle aches experienced by some who take statins.
- Inclirisan (Leqvio), given as a shot twice yearly, blocks production of PCSK9.
- Evinacumab (Evkeeza), a monthly infusion approved only for people with a family history of hypercholesterolemia.
Q: Are there any new tools for calculating an individual’s risk of heart disease?
A: I’ve found the American Heart Association’s new PREVENT calculator to be a convenient resource to assess an individual’s risk of heart attack, stroke or heart failure over the next 10 and 30 years. It’s more comprehensive than earlier versions, as it includes measures of kidney function and metabolic health and can be used to predict risk in patients as young as age 30, which is extremely valuable in terms of early detection.

by Specialdocs Consultants | Aug 20, 2024 | Healthy Aging, Patient News
“I’m having a senior moment.
I’m too old to try that.
I look good for my age.
It’s time to put her/him out to pasture.
These are just aches and pains from old age.
Sweetie, you don’t look a day over 29.
Ok boomer.
There will be a tsunami of aging dependents in the coming decade.”
These oft-used phrases may sound inoffensive but they’re actually examples of ageism, perhaps the only stereotype in America yet to be banished, or even fully recognized. Raising awareness of ageist beliefs as inaccurate at best, and physically and psychologically harmful at worst, is the work of a lifetime for a diverse group of medical and scientific advocates. Why is changing the narrative so important?
Research shows that ageism can influence health through three pathways: psychological, behavioral and physiological. Negative age stereotypes can increase biological markers of stress and may predict detrimental brain changes decades later, while also spurring worse health behavior, such as noncompliance with prescribed medications. A national poll on healthy aging showed those who regularly experienced three or more forms of ageism were less likely to rate their mental health as excellent or very good (61% vs. 80%) and more likely to report symptoms of depression (49% vs. 22%) than those who did not. Additionally, ageism can lead to inequities in healthcare, with age-based exclusions common in clinical trials, and older adults more apt to be left out of screenings, investigations and treatment for mental health issues.
Ageism: A Mental and Physical Toll
What may be most important to appreciate is how the internalizing of age stereotypes by older adults themselves can be an important determinant of health and well-being. Experts have found that negative self-perceptions of aging are associated with a higher prevalence for many of the most frequently seen health conditions among Americans, including heart disease, lung disease, diabetes, musculoskeletal disorders, and injuries, and tend to show more shrinkage of hippocampal volume in the brain. They may also show poorer memory performance and start to walk slower, reinforcing the negative loop around their aging process.
The Power of Positive Aging
Flipping the narrative, however, can result in dramatically improved outcomes. As reported in the Gerontologist, those who have more positive age beliefs live on average 7.5 years longer than those who harbor negative age beliefs. As the researchers noted: “If there were a pill that gave people an extra seven years of life in relatively good health, we would encounter very long lines at the pharmacy.”
The reasons for optimism around aging are based on science, not magical thinking. Consider that steep declines in physical and cognitive abilities are not inevitable parts of aging. According to the Administration on Aging, 80% of adults over 65 are not experiencing a physical or cognitive disability such as hearing impairment or memory loss that impacts their function, and 60% report only moderate or small impairments in their mobility. Procedural memory (e.g. how to ride a bike) is maintained in normal aging, and there is evidence suggesting abstract thinking and metacognition improve.
Challenging the Aging Myth
Despite the stereotype of people becoming more curmudgeonly with age, Manfred Diehl, PhD, a lifespan developmental psychologist, reports the opposite: “The conclusion from several meta-analyses is that in the personality area, we see quite a bit of positive development in terms of becoming socially more mature, with improved coping strategies and more regulation of emotions. Conscientiousness tends to increase at least until the mid-60s, possibly early 70s.”
Most remarkably, ongoing research at the Yale School of Public School by epidemiologist Dr. Becca Levy pointed to the conclusion that beliefs about aging rather than aging itself help explain why some older adults thrive while others do not. Her studies found that adults briefly primed with positive statements about aging showed improvements in their memory, gait speed, and balance that were measurable months later, and further generated increasing confidence in their abilities that endured over years. Additional studies suggest that positive beliefs about aging may protect against dementia, even among those with a high-risk gene.
Changing the Conversation Around Aging
How can we help shift the conversation? Start by increasing awareness of the culture of ageism around us and recognize how it can impact health rather than the actual aging process, encourages Levy.
You may also want to explore how to get involved in organizations that focus on bringing generations together, including:
Generations Over Dinner – A free global initiative to create meaningful experiences and conversations by hosting in-person or virtual multi-generational dinner events.
Generations United– A nonprofit network with a comprehensive database of intergenerational programs across the country.
CoGenerate –A nonprofit organization aiming to bridge generational divides and foster intergenerational collaboration.
When to seek help for mental health
Remember: it is not normal for older adults to be unhappy as they age. Seek help for these treatable medical conditions:
Anxiety
- Panic disorder: Panic attacks or sudden feelings of terror that strike repeatedly
- Obsessive-compulsive disorder: Repetitive, unwanted thoughts or rituals
- Post-traumatic stress disorder (PTSD): Nightmares, depression after a traumatic event
- Phobias: Extreme fear of something that poses little real danger
- Generalized anxiety disorder: Chronic worry about everyday activities
Depression
Feelings of intense sadness that last for weeks or months. Symptoms include:
- No pleasure in everyday activities
- Poor sleep
- Rapid weight gain or loss
- Low energy
- Unable to focus
While grieving a loss may look similar to depression, there are differences. A mix of good and bad days is common when grieving. With depression, feelings of emptiness are constant and don’t improve over time.
Sources:Aging Research Reviews; Breaking the Age Code; Contemporary Clinical Trials, NCOA, Helpguide.org

by Specialdocs Consultants | Aug 20, 2024 | Healthy Aging, Mental Health, Patient News
Defined simply as the final menstrual period, when it is no longer possible for a woman to get pregnant, the current approach to menopause has become increasingly nuanced, recognizing that each individual’s experience varies widely. Many women transition into this stage smoothly with minimal discomfort, but others experience severe vasomotor symptoms such as hot flashes, night sweats, sleep disruption, vaginal dryness, and possibly, “brain fog” and poorer mental health.
The Popularity of Hormone Therapy for Menopause
While hormone therapy (HT) was once routinely prescribed to relieve the symptoms of menopause, this stopped as a result of a large Women’s Health Initiative (WHI) study in 2002 which showed an increased risk of heart attacks, breast cancer, blood clots, and strokes for older postmenopausal females using the estrogen-progestin combination.
However, the pendulum may now be swinging back as subsequent trials that addressed the limitations of the WHI study found hormone therapy – consisting of estrogen for symptom relief and progesterone to protect the uterine lining – may be safer than previously thought. For women under 60 who are less than 10 years out from the start of menopause, an estradiol oral pill or transdermal patch can eliminate symptoms that impact sleep and mood and may decrease the risk for heart disease, diabetes and fractures due to osteoporosis. Progesterone can be taken as a pill, patch or IUD.
Further studies have shown that HT needn’t be routinely discontinued after 10 years for women at low risk for breast cancer and cardiac disease who continue to be challenged by persistent menopause symptoms.
Depression and Menopause
Additionally, new research suggests that despite a long-held association of depression with menopause, women are not universally at risk of depressive symptoms over the transition. For those more vulnerable to depression because of severe sleep disruptions, a long transition through menopause, stressful life events, or a previous history of clinical depression, a combination of psychological interventions and medication is advised. Other studies found estrogen treatment, sometimes with an antidepressant, effective in managing mood-related symptoms.
A Healthy Lifestyle to Mitigate Menopause Symptoms
The renewed acceptance of HT has spurred a reconsideration of our entire approach to menopause with practitioners asking: Can a healthy lifestyle play a key role in mitigating menopause symptoms? Can this passage be navigated successfully with informed, individualized decision-making and social and medical support? In 2024, all signs point to yes.

by Specialdocs Consultants | Feb 7, 2024 | Healthy Aging, Patient News
It’s not yet possible to stop the passage of years, but it might well be within our sights to combat the effects of aging, according to Michael Greger, MD, internationally recognized lifestyle medicine physician, author and nutritionist. Synthesizing years of research on the essential pathways of aging, Dr. Greger believes the process can be slowed down with lifestyle changes, and without pharmaceutical interventions. Below are some of his most interesting findings … please note that we always encourage you to check with your physician for individual guidance before adopting new health recommendations.
 Plant-based eating holds one of the most important keys to slowing biological aging, emphasizes Dr. Greger. Borne out in large studies from the National Institutes of Health/AARP and Harvard, replacing just 3% of daily calories from animal protein with plant protein was associated with a 10% decrease in risk of overall mortality. It may also help prevent Alzheimer’s dementia, an incurable disease. “There is a growing consensus that what is good for our hearts is also good for our heads, and high levels of blood cholesterol are recognized to be a major risk factor for Alzheimer’s. Switching to a healthy, whole foods diet lower in animal fats, eggs and dairy can help prevent arteries in the brain from becoming clogged with atherosclerotic plaque, which is thought to play a role in Alzheimer’s,” he explains. “It may even trump genetics, as seen in Nigeria, where the plant-predominant diet may be the reason for very low rates of Alzheimer’s disease among a population with some of the world’s highest rates of the Alzheimer’s gene. Genes may load the gun, but lifestyle pulls the trigger.” In studies of older adults, the benefits of a diet rich in dark green, leafy vegetables continues to emerge, associated with improvements in the brain’s processing speed and working memory, muscle mass and strength, and potentially helping prevent age-related macular degeneration.
Plant-based eating holds one of the most important keys to slowing biological aging, emphasizes Dr. Greger. Borne out in large studies from the National Institutes of Health/AARP and Harvard, replacing just 3% of daily calories from animal protein with plant protein was associated with a 10% decrease in risk of overall mortality. It may also help prevent Alzheimer’s dementia, an incurable disease. “There is a growing consensus that what is good for our hearts is also good for our heads, and high levels of blood cholesterol are recognized to be a major risk factor for Alzheimer’s. Switching to a healthy, whole foods diet lower in animal fats, eggs and dairy can help prevent arteries in the brain from becoming clogged with atherosclerotic plaque, which is thought to play a role in Alzheimer’s,” he explains. “It may even trump genetics, as seen in Nigeria, where the plant-predominant diet may be the reason for very low rates of Alzheimer’s disease among a population with some of the world’s highest rates of the Alzheimer’s gene. Genes may load the gun, but lifestyle pulls the trigger.” In studies of older adults, the benefits of a diet rich in dark green, leafy vegetables continues to emerge, associated with improvements in the brain’s processing speed and working memory, muscle mass and strength, and potentially helping prevent age-related macular degeneration.
 Activate autophagy, the body’s cellular recycling system, with regular aerobic exercise of moderate intensity, and daily consumption of spermidine, a compound found in foods including: beans, tempeh (made from fermented soybeans), white button mushrooms, mangoes, edamame, green peas, lentil soup, and in its most concentrated form in wheat germ. Also given the green light by Dr. Greger is coffee, for its abundance of polyphenol chlorogenic acid, an antioxidant thought to have a protective effect that is contained in all types of the beverage (decaffeinated, instant, and especially when brewed with a paper filter).
Activate autophagy, the body’s cellular recycling system, with regular aerobic exercise of moderate intensity, and daily consumption of spermidine, a compound found in foods including: beans, tempeh (made from fermented soybeans), white button mushrooms, mangoes, edamame, green peas, lentil soup, and in its most concentrated form in wheat germ. Also given the green light by Dr. Greger is coffee, for its abundance of polyphenol chlorogenic acid, an antioxidant thought to have a protective effect that is contained in all types of the beverage (decaffeinated, instant, and especially when brewed with a paper filter).
 Avoid French fries and chips, urges Dr. Greger, as the toxin acrylamide formed during the frying process may cause inflammation and inhibit autophagy; air fry potatoes instead. Also, put down the salt shaker and opt for salt-free seasonings or substitutes. “Cutting back on sodium appears to effectively make people more than a decade younger in terms of risk of premature death,” he says.
Avoid French fries and chips, urges Dr. Greger, as the toxin acrylamide formed during the frying process may cause inflammation and inhibit autophagy; air fry potatoes instead. Also, put down the salt shaker and opt for salt-free seasonings or substitutes. “Cutting back on sodium appears to effectively make people more than a decade younger in terms of risk of premature death,” he says.
 Minimize fish. Long viewed as a healthy choice, fish have become so contaminated with heavy metals, pesticides and other forever chemicals that despite their omega-3 fatty acids, there’s been a failure to consistently observe its beneficial effects, according to Dr. Greger.
Minimize fish. Long viewed as a healthy choice, fish have become so contaminated with heavy metals, pesticides and other forever chemicals that despite their omega-3 fatty acids, there’s been a failure to consistently observe its beneficial effects, according to Dr. Greger.
 Prevent bone fractures by focusing on strength and balance training. “The majority of age-related risk of bone fractures (85%) is due to falling, not osteoporosis, so addressing muscle loss may be more effective than the current focus on increasing bone mineral density with drugs,” says Dr. Greger. He cites multiple randomized trials showing a combination of resistance exercise to improve lower limb muscle strength and balance training can cut fracture risk nearly in half. And although boosting protein intake has been touted by others, Dr. Greger cautions: “If you put together all the randomized, controlled trials of adding extra protein to the diets of older men and women, you find no evidence that it increases muscle mass or strength, even in those with sarcopenia (excessive age-related muscle loss).”
Prevent bone fractures by focusing on strength and balance training. “The majority of age-related risk of bone fractures (85%) is due to falling, not osteoporosis, so addressing muscle loss may be more effective than the current focus on increasing bone mineral density with drugs,” says Dr. Greger. He cites multiple randomized trials showing a combination of resistance exercise to improve lower limb muscle strength and balance training can cut fracture risk nearly in half. And although boosting protein intake has been touted by others, Dr. Greger cautions: “If you put together all the randomized, controlled trials of adding extra protein to the diets of older men and women, you find no evidence that it increases muscle mass or strength, even in those with sarcopenia (excessive age-related muscle loss).”
Finally, he points to the reassuring fact that adopting just a few simple lifestyle behaviors – a diet rich in fruits and vegetables, maintaining a healthy weight, not smoking – adds years of life no matter when you begin. “A Harvard analysis of more than 100,000 men and women followed over decades showed that starting to eat and live more healthfully at age 50 appeared to translate into 12 to 14 years of extra lifespan, at age 60, an extra 8 to 9 years, and even starting at age 80 added more years. We all have the power to turn back the clock, starting right now.”
Eight Lessons from the Blue Zones
Blue Zones are areas across the globe in which populations live longer and better than average, identified by National Geographic fellow Dan Buettner, who explains: “There’s no magic bullet or pill, but rather a cluster of mutually supporting factors common to these centuries-old cultures whose people are making it to ages 90-100 without disease.”
- Plant-slant diet, as described elsewhere in this issue. Buettner’s common sense advice: “Sit down with a plant-based cookbook, identify a dozen recipes that you think your family would enjoy and cook them instead of going on a diet or spending money on a program. Also, eliminate soda pop, one of the unhealthiest parts of the American diet.”
- Eat until you’re 80% full. “And have your biggest meal first,” advises Buettner, “eat breakfast like a king, lunch like a prince and dinner like a pauper.”
- Family-first focus.
- Belonging: feeling connected to your community.
- Right tribe: surrounded by friends who support healthy behaviors.
- Natural movement throughout the day.
- Strong sense of purpose.
- Ability to de-stress.
The original Blue Zones ranged from Costa Rica to Sardinia. According to new research, these states closer to home are most likely to earn the moniker in the future: California, Minnesota, Utah, North Carolina, Massachusetts, Maryland, Virginia, Connecticut, Rhode Island, Colorado.

by Specialdocs Consultants | Apr 14, 2023 | Healthy Aging, Medications, Nutrition, Patient News
The aching, swollen, stiff joints associated with osteoarthritis (OA) have long been considered a “wear and tear” condition, associated with aging. It was thought that cartilage, the smooth connective tissue on the end of bones that cushion the joints, simply breaks down over a lifetime of walking, exercising and moving. New research shows that it is a disease of the entire joint that also causes bony changes of the joints, deterioration of tendons and ligaments and inflammation of the synovium (lining of the joint). While more prevalent in people over 50, OA can show up in younger patients, especially those who’ve experienced a joint injury such as a torn ACL or meniscus. The promising news is that according to the Arthritis Foundation, “OA is not an inevitable aging disease” and the Cleveland Clinic notes: “Age is a contributing factor, although not all older adults develop osteoarthritis and for those who do, not all develop associated pain.”
Still, currently OA is by far the most prevalent form of arthritis, affecting more than 32.5 million Americans, and primarily targeting knees, hips, hands and spine. A variety of factors contribute to the development of OA, including congenital joint deformity, family history, previous joint injury, and years of physically demanding work or contact sports. However, reducing risk is possible with attention to these modifiable factors:
- Obesity adds stress and pressure to joints. Consider that your knees bear a force equivalent to three to six times your body weight with each step, so a lighter weight relieves the burden considerably – losing one pound takes 3 pounds off the knees.
- Lifestyle. Being physically active is crucial, as a sedentary lifestyle and obesity are associated with a higher risk of OA. While sports such as football, baseball and soccer may pose a risk because of their impact on joints, most types of regular or moderate exercise can be safely done.
Living with Osteoarthritis
Unfortunately, there is no cure for OA, and managing symptoms such as joint stiffness, tenderness, swelling, and popping or crackling can become increasingly difficult over time. While seeking a pill to alleviate discomfort is a natural reaction, consider trying alternative solutions to help break the cycle of chronic pain.
“The longer the brain processes pain, the more hypersensitive it becomes to pain,” explains Rachel Welbel, MD, a physiatrist who is extensively trained in physical medicine and rehabilitation and sports medicine. “The brain, now constantly on high alert, may respond to non-painful sensations as if they are painful. Poor diets and stress can increase chemicals in the brain that reinforce this response, prolonging the pain cycle.”
Reflecting a more holistic and multi-faceted approach to managing pain, she says: “Opioids are almost never the answer.” Instead, she recommends lifestyle modifications, treatments and medications that help tackle pain in a variety of ways.
Lifestyle Modifications, Treatments and Medications for Osteoarthritis
Weight management. Obesity is not only a leading risk factor for OA, but adds to the pain for those with the condition. Body fat produces proteins called cytokines that cause inflammation, and in the joints, can alter the function of cartilage cells. Shedding even a few pounds can make a difference: losing just 10% of your body weight can cut arthritis pain in half, and losing another 20% can reduce the pain by an additional 25% or more, and may slow or even halt progression of the disease.
Exercise and movement. “Exercise is key to living well with OA,” says Welbel. “While resting aching joints may bring temporary relief, lack of movement ultimately leads to more discomfort. The focus is not on weight loss but on minimizing pain and maximizing strength.” Plan on 150 minutes of light to moderate exercise each week. She recommends working with a physical therapist who can analyze your joint biomechanics and suggest exercises to strengthen muscles and improve range of motion while reducing stiffness and pain. “In addition, exercise is a natural mood elevator,” says Welbel. “Walk, swim, or try mindfulness-based, stress-reducing exercise such as yoga and tai chi.”
Anti-inflammatory diet. Increasing consumption of fruits, vegetables, whole grains, legumes and fish, while reducing consumption of red and processed meats, refined grains, and sugar-containing beverages and foods, may play an important role in reducing pain associated with inflammation from OA, says Welbel. Try incorporating into your diet fatty fish; herbs and spices such as garlic, turmeric and cinnamon; yogurt and other fermented foods; and healthy fats such as avocados, extra virgin olive oil and walnuts.
Supportive devices. A cane or walker can help lighten the load on your joints, decrease pain, and reduce your risk of falling. Intermittent use of a knee brace may be helpful for added stability, especially if walking on uneven surfaces. Foot orthotics such as arch supports and metatarsal pads may reduce foot pain.
Medications. Over-the-counter (OTC) pain relievers like acetaminophen (Tylenol) may help joint pain and stiffness for some. Nonsteroidal anti-inflammatory drugs (NSAIDs) are also used to relieve pain, including OTC medications such as Advil or Aleve, or Celebrex, a prescription medication with a somewhat lower risk of ulcers and upper gastrointestinal bleeding than other NSAIDs. Topical NSAIDS such as Aspercreme and other creams or patches containing ingredients such as capsaicin, menthol or lidocaine can help.
Injections. Corticosteroids injections may provide temporary relief for acute flare-up of OA pain in knees and finger joints, but effectiveness can vary, and you must wait at least 3 to 6 months to repeat an injection in a specific joint if needed. Viscosupplementation involves injection of a gel-like substance containing hyaluronic acid, which acts as a lubricant in the fluid between bony surfaces and is decreased in OA joints. Research results for significant pain reduction or improved function are not yet convincing, but there appear to be a number of patients with mild to moderate knee OA who report symptom relief.
Supplements. Research results are mixed, but we note some of the more well-known supplements with the caution that these are not recommended to be used alone as treatments for OA. Glucosamine and chondroitin sulfate, naturally occurring compounds found in healthy cartilage, may help reduce joint pain and stiffness, and have been available in the U.S. and Europe for several decades. Other supplements such as tart cherry and turmeric may help reduce OA symptoms for some.
Other promising but not yet proven treatments. Platelet-rich plasma (PRP) injections and stem cell therapy have been used to treat pain of mild to moderate knee OA, but evidence of effectiveness is mixed, and these are still considered experimental. Elements of Eastern medicine, including herbs and acupuncture, may help control OA symptoms, but have not yet been confirmed in large clinical studies.
A Generation of Joint Replacements
When diet and exercise modifications, supportive devices, medications and injections no longer sufficiently ease the pain of OA, a hip or knee replacement may be recommended. The number of people opting for this surgery increases each year, now totaling more than 790,000 knee and 450,000 hip replacements annually.
The implants, made of plastic, metal or ceramic, are traditionally kept in place with bone cement, which is gradually being replaced by newer cementless and porous titanium systems to improve bone fixation and durability. Also on the rise is computer-assisted surgery to increase placement accuracy of the prosthetic components, and patient-specific implants using 3D printing technology. The combination of modern materials and advanced surgical techniques have extended the durability of most implants to 20 years, a marked improvement over the previous standard of 10 to 15 years.
Recovery time has also changed for the better. With rehabilitation to regain strength and motion, normal activities can usually be resumed within weeks to months. Most importantly, the majority of patients are highly satisfied with the results, reporting minimal to no pain and significantly improved function and quality of life. However, outcomes can vary and potential complications should be discussed before proceeding.
Additional breakthroughs may be on the horizon: researchers at Duke University start trials this spring of a hydrogel-based cartilage substitute that may prove more durable than natural cartilage…stay tuned!
Every patient is unique…please check with your healthcare provider to discuss recommendations for prevention and treatment based on your individual health situation.
Sources: Arthritis Foundation, AAOS, Orthoworld, Cleveland Clinic, National Academy of Medicine (formerly Institute of Medicine), UpToDate, US Department of Agriculture, American College of Rheumatology.





 Plant-based eating holds one of the most important keys to slowing biological aging, emphasizes Dr. Greger. Borne out in large studies from the National Institutes of Health/AARP and Harvard, replacing just 3% of daily calories from animal protein with plant protein was associated with a 10% decrease in risk of overall mortality. It may also help prevent Alzheimer’s dementia, an incurable disease. “There is a growing consensus that what is good for our hearts is also good for our heads, and high levels of blood cholesterol are recognized to be a major risk factor for Alzheimer’s. Switching to a healthy, whole foods diet lower in animal fats, eggs and dairy can help prevent arteries in the brain from becoming clogged with atherosclerotic plaque, which is thought to play a role in Alzheimer’s,” he explains. “It may even trump genetics, as seen in Nigeria, where the plant-predominant diet may be the reason for very low rates of Alzheimer’s disease among a population with some of the world’s highest rates of the Alzheimer’s gene. Genes may load the gun, but lifestyle pulls the trigger.” In studies of older adults, the benefits of a diet rich in dark green, leafy vegetables continues to emerge, associated with improvements in the brain’s processing speed and working memory, muscle mass and strength, and potentially helping prevent age-related macular degeneration.
Plant-based eating holds one of the most important keys to slowing biological aging, emphasizes Dr. Greger. Borne out in large studies from the National Institutes of Health/AARP and Harvard, replacing just 3% of daily calories from animal protein with plant protein was associated with a 10% decrease in risk of overall mortality. It may also help prevent Alzheimer’s dementia, an incurable disease. “There is a growing consensus that what is good for our hearts is also good for our heads, and high levels of blood cholesterol are recognized to be a major risk factor for Alzheimer’s. Switching to a healthy, whole foods diet lower in animal fats, eggs and dairy can help prevent arteries in the brain from becoming clogged with atherosclerotic plaque, which is thought to play a role in Alzheimer’s,” he explains. “It may even trump genetics, as seen in Nigeria, where the plant-predominant diet may be the reason for very low rates of Alzheimer’s disease among a population with some of the world’s highest rates of the Alzheimer’s gene. Genes may load the gun, but lifestyle pulls the trigger.” In studies of older adults, the benefits of a diet rich in dark green, leafy vegetables continues to emerge, associated with improvements in the brain’s processing speed and working memory, muscle mass and strength, and potentially helping prevent age-related macular degeneration. Activate autophagy, the body’s cellular recycling system, with regular aerobic exercise of moderate intensity, and daily consumption of spermidine, a compound found in foods including: beans, tempeh (made from fermented soybeans), white button mushrooms, mangoes, edamame, green peas, lentil soup, and in its most concentrated form in wheat germ. Also given the green light by Dr. Greger is coffee, for its abundance of polyphenol chlorogenic acid, an antioxidant thought to have a protective effect that is contained in all types of the beverage (decaffeinated, instant, and especially when brewed with a paper filter).
Activate autophagy, the body’s cellular recycling system, with regular aerobic exercise of moderate intensity, and daily consumption of spermidine, a compound found in foods including: beans, tempeh (made from fermented soybeans), white button mushrooms, mangoes, edamame, green peas, lentil soup, and in its most concentrated form in wheat germ. Also given the green light by Dr. Greger is coffee, for its abundance of polyphenol chlorogenic acid, an antioxidant thought to have a protective effect that is contained in all types of the beverage (decaffeinated, instant, and especially when brewed with a paper filter). Avoid French fries and chips, urges Dr. Greger, as the toxin acrylamide formed during the frying process may cause inflammation and inhibit autophagy; air fry potatoes instead. Also, put down the salt shaker and opt for salt-free seasonings or substitutes. “Cutting back on sodium appears to effectively make people more than a decade younger in terms of risk of premature death,” he says.
Avoid French fries and chips, urges Dr. Greger, as the toxin acrylamide formed during the frying process may cause inflammation and inhibit autophagy; air fry potatoes instead. Also, put down the salt shaker and opt for salt-free seasonings or substitutes. “Cutting back on sodium appears to effectively make people more than a decade younger in terms of risk of premature death,” he says. Minimize fish. Long viewed as a healthy choice, fish have become so contaminated with heavy metals, pesticides and other forever chemicals that despite their omega-3 fatty acids, there’s been a failure to consistently observe its beneficial effects, according to Dr. Greger.
Minimize fish. Long viewed as a healthy choice, fish have become so contaminated with heavy metals, pesticides and other forever chemicals that despite their omega-3 fatty acids, there’s been a failure to consistently observe its beneficial effects, according to Dr. Greger. Prevent bone fractures by focusing on strength and balance training. “The majority of age-related risk of bone fractures (85%) is due to falling, not osteoporosis, so addressing muscle loss may be more effective than the current focus on increasing bone mineral density with drugs,” says Dr. Greger. He cites multiple randomized trials showing a combination of resistance exercise to improve lower limb muscle strength and balance training can cut fracture risk nearly in half. And although boosting protein intake has been touted by others, Dr. Greger cautions: “If you put together all the randomized, controlled trials of adding extra protein to the diets of older men and women, you find no evidence that it increases muscle mass or strength, even in those with sarcopenia (excessive age-related muscle loss).”
Prevent bone fractures by focusing on strength and balance training. “The majority of age-related risk of bone fractures (85%) is due to falling, not osteoporosis, so addressing muscle loss may be more effective than the current focus on increasing bone mineral density with drugs,” says Dr. Greger. He cites multiple randomized trials showing a combination of resistance exercise to improve lower limb muscle strength and balance training can cut fracture risk nearly in half. And although boosting protein intake has been touted by others, Dr. Greger cautions: “If you put together all the randomized, controlled trials of adding extra protein to the diets of older men and women, you find no evidence that it increases muscle mass or strength, even in those with sarcopenia (excessive age-related muscle loss).”
Recent Comments