
by Specialdocs Consultants | Apr 14, 2023 | Healthy Aging, Medical Conditions, Medications, Nutrition, Patient News
Except for dedicated thespians, saying “break a leg” is most definitely not a harbinger of good luck. More than 10 million Americans are living with osteoporosis, a condition of low bone mass that results in increased risk of bone fracture, sometimes even from a minor fall or pressure from a big hug. Over 1.5 million osteoporotic fractures occur annually, and 1/3 of women and 1/5 of men over 50 will experience an osteoporotic bone fracture in their lifetime. The good news is that reliable diagnostic testing and treatments are available, which we share below.
Who’s at Risk for Osteoporosis?
Osteoporosis is sometimes referred to as a “silent disease” because it is painless unless a fracture occurs, so people often are unaware they have it until that happens. Post-menopausal women are at highest risk, in part due to the decline in estrogen levels. Estrogen, and to an even greater extent, testosterone, are hormones that help ward off osteoporosis, which is why it is not as common in men. Others at risk include those with autoimmune diseases such as rheumatoid arthritis and celiac disease, those with high parathyroid or thyroid levels and certain other chronic diseases.
Medications including corticosteroids, proton pump inhibitors and certain antidepressants and anti-seizure medications may increase risk of bone thinning. Inherited factors may affect risk, such as race (more common in Caucasians and Asians), body shape and size (smaller/thinner individuals more at risk) and family history of osteoporosis. Physical activity level and diet play a role, placing those who are sedentary and/or have a diet low in calcium at higher risk. Cigarette smoking and higher alcohol intake are also risk factors.
How Osteoporosis is Diagnosed
A bone density measurement test is the best way to diagnose osteoporosis, using the DEXA (dual energy x-ray absorptiometry) scan of hip and spine. The severity of decrease in bone mass is determined by your T-score: Between -1.0 and -2.5 is defined as osteopenia, when bones are weaker than normal, while -2.5 or less indicates osteoporosis.
Osteoporosis Medications
A number of medications are available to treat osteoporosis.
- Bisphosphonates to slow the breakdown and removal of bone are typically tried first. Fosamax, used most, is a weekly pill often taken for 5 years followed by a “drug holiday.” The IV bisphosphonate Reclast is generally continued for three years.
- Evista is a daily pill for post-menopausal osteoporosis that protects against bone loss and also reduces the risk of breast cancer in high-risk women.
- Prolia is injected every 6 months to slow breakdown and removal of bone and help increase bone density. It should not be discontinued once started or must be followed by another medication if stopped.
- Evenity is injected once a month for a year to increase new bone and reduce breakdown and removal of bone.
- Forteo and Tymlos are drugs that help build bone for people at high risk of fracture. These are injected daily for two years.
Managing Osteoporosis
Peak bone mass is achieved by age 25-30 years, but at any age, a healthy lifestyle can aid in strengthening bones. Focus on eating a balanced diet rich in vitamin D and calcium (see sidebar), and remember that exposing the body to natural sunlight increases production of vitamin D. Eliminating tobacco use and limiting alcohol is strongly recommended to promote maximum absorption of calcium and vitamin D. Taking fall prevention measures is crucial: consider that 95% of hip fractures are caused by falls.
Aim for 30 minutes of weight-bearing and muscle strengthening exercises on most days:
- Walk or run on level ground or a treadmill
- Dance
- Climb stairs
- Lift weights without straining your back
- Sit-to-stand exercises: start with an elevated seat height, and progress to a lower chair as you get stronger
- Strengthen thighs: stand against a wall and slide down into a slight knee bend, hold for 10 seconds and repeat a few times
- Tai Chi: combines slow movements, breathing exercises, and meditation
Nourishment Know-How for Bone Health
For optimal bone health, a daily intake of 1200-1500 mg of calcium and 400-800 IU (international units) of Vitamin D is recommended for adults. In many cases, supplementation may be appropriate.
Selected sources with calcium and/or Vitamin D:
- Dairy products
- Calcium- and vitamin D-fortified foods and beverages (soy or almond milks, cereals, cheese)
- Dark green, leafy vegetables
- Fish such as salmon, trout, mackerel, tuna, sardines
- Egg yolks
- Sesame or chia seeds, figs, almonds
Fall Prevention Measures for Those with Osteoporosis Include:
- Avoid ladders, step-stools and roof work
- Eliminate tripping hazards like throw rugs, obstacles or cords on the floor
- Be careful around pets and leashes
- Use good lighting, night lights, update glasses and eye care to optimize vision
- Stay fit with regular strengthening and balance exercises
- Wear non-slip shoes
- Install handrails and grab bars in the bathroom
Every patient is unique…please check with your healthcare provider to discuss recommendations for prevention and treatment based on your individual health situation.
Sources: Arthritis Foundation, AAOS, Orthoworld, Cleveland Clinic, National Academy of Medicine (formerly Institute of Medicine), UpToDate, US Department of Agriculture, American College of Rheumatology.

by Specialdocs Consultants | Jan 17, 2023 | Healthy Aging, Patient News
The growing group of people able to enjoy 100 years of life may well be one of the most remarkable achievements of the 21st century. A generation ago, the number of centenarians worldwide was just 110,000; today they are 600,000 strong. Notably, a sizable segment of this long-lived group, aptly called Super Agers, reach 100 in good health with no age-related disease or disability. Are they the fortunate recipients of outstanding genes, followers of a particularly healthy lifestyle, or a combination of both?
Definitive answers may start to emerge sooner than we had imagined possible, thanks to the SuperAgers Family Study, called one of the most ambitious ever conducted, with the goal to uncover and understand the genetic and biological mysteries of exceptional longevity and healthy aging. The initiative, spearheaded by the American Federation for Aging Research (AFAR) and Albert Einstein College of Medicine, in collaboration with https://www.bumc.bu.edu/busm Boston University School of Medicine, will recruit 10,000 people over age 95 to collect their DNA samples and health histories, as well as their children’s.
“Super Agers show us that chronic disease is not an inevitable part of aging, and that an extended period of good health can accompany a long lifespan,” says Sofiya Milman, MD, principal investigator of the study and director of Human Longevity Studies at Einstein’s Institute for Aging Research.
While previous research has attempted to pinpoint the distinctive characteristics of people living well in their ninth and tenth decades, the enrollment of 10,000 participants in SuperAgers will represent the largest cohort ever studied. The extensive numbers are essential to obtaining meaningful data that can benefit many in the future, according to Milman.
“We believe longevity may be linked to rare genetic variants found in less than five percent of the population, making it a challenge to amass ample genetic evidence,” explains Milman. “The enormous data bank being built in our SuperAgers study will enable us to identify these genes, understand their biological pathways and explore how to duplicate their functions.”
Milman aims to achieve full enrollment over the next two to three years, with results from the first phase available in 2024. “SuperAgers will significantly accelerate our research by providing us with a treasure trove of data on not just genetics, but biological and behavioral factors that affect aging and its related diseases. Ultimately, this will help us develop, trial and fast-track new therapies to extend a healthy old age,” she says.
In the meantime, adhering to a nutritionally balanced diet, exercising, getting sufficient sleep, managing stress and eliminating tobacco are all well advised. “A healthy lifestyle alone may not be enough to guarantee you reach 100,” admits Milman, “but all evidence points to the fact that it will extend your healthy lifespan.”
SuperAgers Sign-Up
Interested in being part of the SuperAgers family study?
Individuals who have passed their 95th birthday, as well as children of those individuals, are invited to enroll online at http://www.superagersstudy.org and complete a health history, family history and demographic profile. Those eligible will receive a biospecimen collection kit in the mail and are asked to return it in a postpaid envelope to the Albert Einstein College of Medicine, which will store and process each participant’s DNA. Please note that participants may choose to receive results regarding their ancestry or family origins. The SuperAgers biobank holding the DNA records, and all the related data, will be protected and maintained at Einstein in compliance with federal medical privacy law (HIPAA).


by Specialdocs Consultants | Oct 6, 2022 | Healthy Aging, Patient News, Wellness
Senior Moments Or Something More?
As Baby Boomers continue the inexorable journey deep into their senior years, preserving cognitive function understandably tops the list of worries. While Alzheimer’s Disease and related dementias are seen in just 5% of people over 65, that number jumps to 30% for people age 85 and over. Questions abound: is forgetting a name a sign of normal aging or an indicator of a more serious memory disorder? Are any nutritional supplements or pharmaceutical treatments available that are proven to stave off memory loss? Most importantly, what steps can be taken to modify individual risk?
To better understand how to identify and manage dementia and Alzheimer’s disease, we asked one of the country’s leading experts, R. Sean Morrison, MD, for his informed perspective on this growing concern for seniors, their families and caregivers. A practicing geriatrician, palliative medicine physician and health researcher for almost three decades, Dr. Morrison has earned numerous awards and recognition for his work, and currently serves as the Chair of the Brookdale Department of Geriatrics and Palliative Medicine at the Icahn School of Medicine at Mount Sinai and as Director of the Hertzberg Palliative Care Institute.
 Is memory loss an inevitable, natural sign of aging?
Is memory loss an inevitable, natural sign of aging?
Dr. Morrison: The good news is that not all cognitive functions decline with age. The ability to maintain attention, language comprehension, usage, and vocabulary does not decrease. Knowledge learned years ago like how to ride a bike, or brush your teeth, also stays intact. Additionally, when you learn something new and can remember it, you won’t forget it any more rapidly than when you were younger.
The not so good news is that it will take greater effort to learn those new things; more attention, repetition and use of memory-enhancing strategies will be needed. The ability to multitask is also diminished, as processing information takes longer and reaction times are slower. People may experience poorer performance when working under time pressure, and find it more difficult to manipulate information in the brain, such as calculating a tip in a restaurant or figuring out a route to travel from one place to another.
 How do you distinguish between a “senior moment” lapse in memory and a sign of Alzheimer’s disease?
How do you distinguish between a “senior moment” lapse in memory and a sign of Alzheimer’s disease?
Dr. Morrison: So many people experience that temporary inability to remember a name. But if you are able to recall things with a cue or can pick it out from a list of possibilities, that’s evidence of a problem with retrieval but not with storage. You can be reassured that it doesn’t indicate Alzheimer’s disease but a “senior moment” because the information has been successfully stored in your memory.
 Is routine screening for dementia recommended in older adults?
Is routine screening for dementia recommended in older adults?
Dr. Morrison: The U.S. Preventive Services Task Force does not recommend for or against routine screening, saying no interventions are proven to have a significant effect in people with earlier detected cognitive impairment. However, it is required as part of Medicare’s yearly assessments, and most primary care physicians consider dementia screenings an essential part of their annual wellness exam.
 What types of screening tests do you recommend?
What types of screening tests do you recommend?
Dr. Morrison: At least a dozen tests are available, each with their own benefits and drawbacks. I recommend the following for their ease of use and proven sensitivity and specificity in diagnosing cognitive impairment:
- Mini-Cog is a quick, three-minute evaluation. Patients are asked to repeat three words, draw a clock with hands at a specific time, and then recall the initial three words.
- Memory Impairment Screen assesses free and cued word recall. Patients are read four unrelated words from four categories (e.g. Red Cross, saucer, checkers, telegram) and after a few minutes of diversion, asked to recall the words in 20 seconds, either with no prompting or cued by category.
- Animal Fluency Test. Patients are asked to name as many animals as possible in a 60-second period.
 Are there any risk factors for dementia and Alzheimer’s disease that can be controlled by patients?
Are there any risk factors for dementia and Alzheimer’s disease that can be controlled by patients?
Dr. Morrison: Quite a few risk factors are modifiable with lifestyle changes and non-pharmaceutical treatments. These include:
- Address hearing and visual impairments, with eyeglasses, hearing aids and other assistance
- Prevent and manage hypertension and diabetes
- Maintain a healthy weight
- Stop smoking
- Seek treatment for depression
- Prioritize regular exercise and physical activity
- Avoid social isolation
- Explore cognitive training
The best advice I can give to people in their 50s to 70s looking to prevent or delay progression of dementia and Alzheimer’s disease: exercise, exercise, exercise and rigorously control your blood pressure.
 How are the symptoms frequently experienced by people with dementia – sleep disturbance, mood disorders, agitation – best addressed?
How are the symptoms frequently experienced by people with dementia – sleep disturbance, mood disorders, agitation – best addressed?
Dr. Morrison: There are a number of non-pharmaceutical interventions that have proven effective. Use adaptive clothing and assistive devices to help eliminate distress around bathing and dressing. Create a reassuring familiar structure to the day with a regular routine and activities. Optimize the sleep environment with a comfortable temperature, the right amount of light, a warm milky drink and a bath or shower before bed; avoid stimulating medications, drinks containing caffeine and alcohol, and exercise too close to bedtime. Pharmaceutical treatments can also be considered, including antidepressants to improve cognition and ameliorate agitation and aggression, and melatonin and melatonin antagonists to help with sleep disorders. Of note: medications such as benzodiazepines (BZD), non-BZD hypnotics, mood stabilizers and antipsychotics are no longer routinely recommended as side effects can outweigh possible benefits.
 Are there any benefits to nutritional supplements or appetite stimulants?
Are there any benefits to nutritional supplements or appetite stimulants?
Dr. Morrison: Nutritional supplements can help with weight gain in patients with anorexia or cachexia (‘wasting’ syndrome) but have no meaningful impact on survival. And while appetite stimulants such as cannabinoids and steroids are often given to help patients with dementia, there is no consistent data regarding their safety and efficacy.
 What medications are available to treat or stop the progression of dementia?
What medications are available to treat or stop the progression of dementia?
Dr. Morrison: Until last year, only four medications were approved for treatment of dementia and Alzheimer’s disease, showing only a minimal to modest improvement in cognition. In 2021 a fifth drug was launched – aducanumab – a monoclonal antibody designed to reduce amyloid protein in the brain. Its fast-track approval was quite controversial as the clinical benefits of the drug were not proven during trials, which were stopped early as a result, and some severe side effects were observed. Interestingly, some researchers are now rethinking the idea that targeting amyloid protein plaques will eliminate Alzheimer’s disease, and instead exploring Alzheimer’s as a disease of inflammation. This could be the next fascinating line of research.
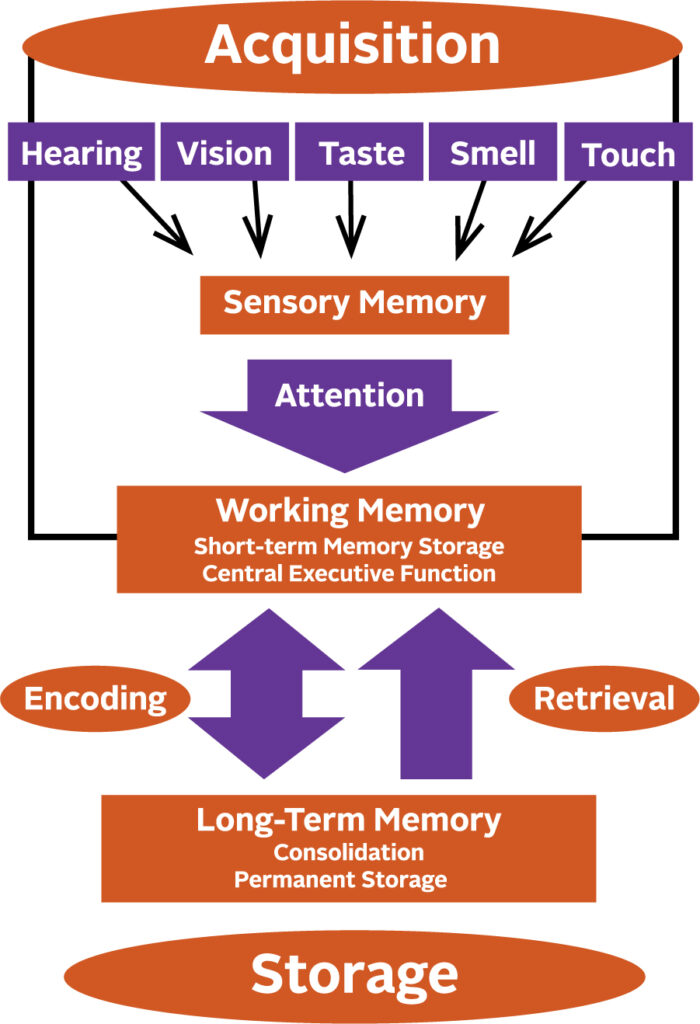
How a Memory is Made
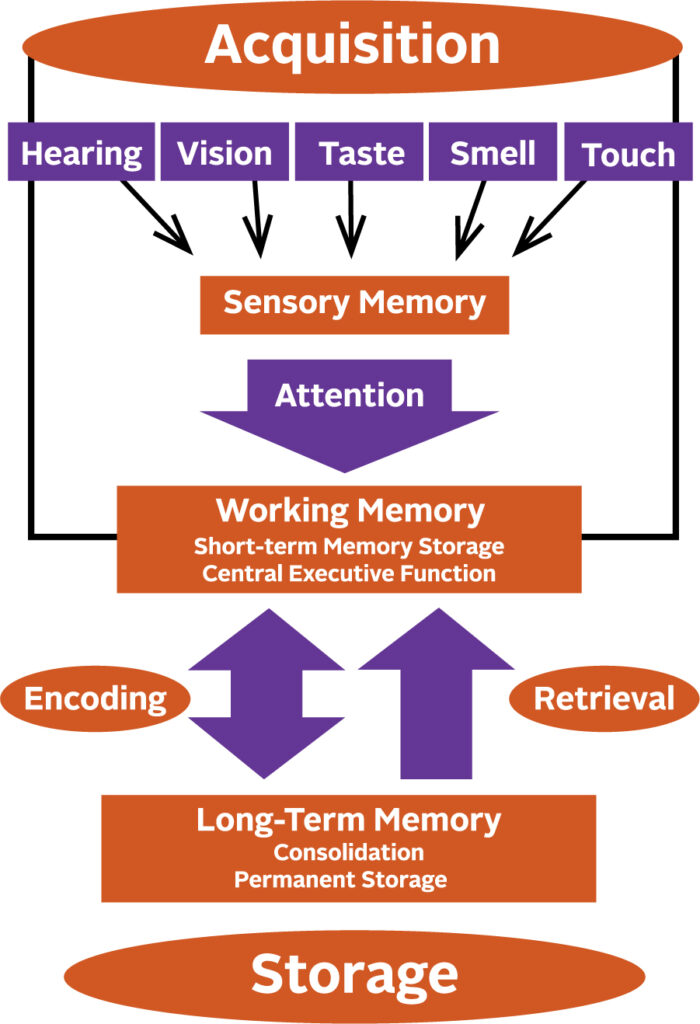
Memory begins to form by giving attention to the information received through your senses. Anything that interferes with your ability to pay attention, such as hearing impairment, will affect the formation of a sensory memory. Successful integration of sensory memories into your working memory enables you to temporarily store, organize and manipulate information. These memories are then encoded into long-term memory and finally put into permanent storage.

by Specialdocs Consultants | Jul 8, 2022 | Healthy Aging, Patient News, Staying Active
Try Pickleball, the Country’s Fastest-Growing Sport
Tired of the same ‘ole routine every summer but find yourself in a pickle and looking for a new summer activity? Well, according to American Council on Exercise (ACE), you might want to consider pickleball.
As everyone from your next-door neighbor to ACE will attest, pickleball is extraordinarily popular. Its rapid rise to ubiquity can be attributed to a number of factors, ranging from easily learned rules and minimal equipment needs to intergenerational appeal and abundant opportunities for socializing.
This blend of badminton, tennis and table tennis can be adjusted to suit the intensity and competitiveness of the players, making it simple enough for beginners but fast-paced enough for more fit or skilled participants.
All of which is to say that if you haven’t yet considered picking up a pickleball paddle and the light, whiffle-like plastic ball, summer 2022 might be the perfect time to do so.
“Pickleball doesn’t require the skill of tennis, so it is easily adapted by most, and provides all the benefits of movement, including calorie burning and enhanced functional capabilities,” says Dr. Cedric Bryant, ACE president and chief science officer.
Already a favorite sport in retirement communities, pickleball has swelled to include more than 4.8 million players in the U.S. – almost double the number from five years ago – earning it the title of fastest-growing sport in 2021 and 2022. According to the Sports and Fitness Industry Association, the spike has been fueled by people ages 54 and younger looking for a friendly yet competitive and lively sport.
“People who play are generally having so much fun they don’t realize how much exercise they’re actually getting,” says Laura Gainor, spokesperson for the USA Pickleball Association.
At 44 x 20 feet, the pickleball court is one quarter the size of a tennis court, so it’s easier to keep the ball in play and achieve a brisk workout. According to ACE, pickleball may provide just what many middle-aged and senior adults are seeking – a safe and effective workout that yields long-term benefits and encourages lifelong participation.
A small research study recently conducted by the organization among people ages 40 to 85 showed that playing four 15-minute pickleball matches three days each week meets exercise intensity guidelines for improving and maintaining cardiorespiratory fitness. Study authors reported the positive impact on cardiometabolic risk factors, with participants experiencing favorable changes in cholesterol levels, systolic and diastolic blood pressure, and peak oxygen uptake after six weeks.
The smaller court also benefits older people or those who have problems with their joints, because less running is needed, resulting in less wear and tear on the joints. One cautionary note: Experts advise learning proper technique to prevent falls. As always, be sure to check with your healthcare provider before beginning any new physical activity.
“Take a few lessons to get started, and you’ll quickly ramp up,” assures Gainor. “After three to five games, you’ll have a very good understanding of how to play, and will become addicted to it shortly after!”
Take It Outside: Keep Moving This Summer
There’s no one-sport-fits-all approach, so if pickleball doesn’t appeal, find your inspiration in one of these activities, spanning the spectrum from low exertion to highly energetic:
- Stroll through farmers’ markets or art fairs
- Go produce picking at a local orchard
- Forest bathe – immerse yourself in nature at a forest preserve
- Gardening – remember to bend from your knees and waist rather than your back
- Swim – use a variety of strokes to limber up your whole body
- Disc golf – a low-impact way to challenge your coordination
- Yard yoga – take your mat and routine outdoors
- Hike, jog, run or cycle on an outdoor trail
- Kayaking – for a vigorous upper body workout
- Stand-up paddleboarding or Boga – challenging, board-based water workouts
Sources: American Council on Exercise, American Heart Association, USA Pickleball Association
by Ivan | Nov 26, 2019 | Healthy Aging, Patient News, Wellness

Life’s Happiness Continuum
Is there a predetermined peak age for happiness, before which our normal outlook is gloomy and melancholy and after which we slump back into these non-euphoric ways? When Are the Best Years of Our Lives?
Studies Show Two Stages of Life Happiness
Like trying to define why some people are born to be joyful and others to play the role of curmudgeon, this issue has long intrigued psychological and social science researchers. While no singular conclusion has been reached, there are a number of compelling hypotheses…and you may be pleasantly surprised to learn that a number of studies suggest a U-shaped happiness curve with peaks for young and old, giving us not one but two stages of life to savor. Mid-life can be stressful, full of the challenges and demands of raising a family and sustaining a career, but according to some experts, there is indeed a light at the end of the tunnel.
The Economist’s international survey of happiness gathered data from America’s General Social Survey, Eurobarometer and Gallup finding an upward trajectory of happiness until age 30, a downward trend into midlife, with the lowest point reached at age 46, and up to higher levels again after the 50’s. Jonathan Rauch, a senior fellow at the Brookings Institution and author of the 2018 book, The Happiness Curve, says although its effects vary between individuals, there appears to be a subtle but insistent tug that makes happiness more difficult to achieve in midlife and then reverses direction when we least expect it.
Other research supports this finding, including a University of Chicago retrospective study of 28,000 Americans over a 32-year period which showed older age groups were consistently the happiest. Interestingly, Dr. Dilip Jeste, director of the UC San Diego Center for Healthy Aging, describes it not as a curve, but more of a linear improvement in mental health that occurs even as physical and cognitive function declines.
Might Happiness in Women Peak Between the Ages of 50-70?
In particular, today’s women may find some of their sweetest times between ages 50 and 70, according to an in-depth lifestyle study spanning three decades conducted by the TrendSight Group. The take-away for younger generations: “Aging isn’t a dirty word, with it can come incredible confidence, strength and freedom,” says study author Marti Barletta. Even better, a full 59% of women ages 50 to 70 felt their greatest achievements were still ahead of them.
Happiness may Increase with Age
Experts theorize a number of reasons that happiness may increase with age, including increased wisdom or psychological intelligence in handling challenges, fewer aspirations and expectations of self, greater appreciation for life, living in the moment with less worry about the future, greater ability to regulate emotions and less worry about pleasing everyone all the time. Stanford psychologist Laura Carstensen’s Socioemotional Selectivity Theory, which is grounded in the unique human ability to monitor time, suggests that relative to younger people, older adults focus more on positive than negative information and prioritize emotionally meaningful activities – notably, deepening close relationships – over those related to individual achievement and exploration.
Recent findings from the Harvard Study of Adult Development, one of the world’s longest studies of adult life, begun in 1938, also point to the vital role of relationships in happiness at older ages. According to the research, these ties protect people from life’s discontents, help to delay mental and physical decline, and are better predictors of long and happy lives than social class, IQ or genes. Dr. Robert Waldinger, study director and psychiatrist at Massachusetts General Hospital, acknowledges that the research shows correlation, not necessarily causation. However, after following the subjects (including both Harvard graduates and inner-city residents) for many decades and comparing the state of their health and their relationships early on, he is confident that strong social bonds play a causal role in long-term well-being.
Perhaps 19th century journalist David Grayson had the best advice of all: “The other day a man asked me what I thought was the best time of life. ‘Why,’ I answered without a thought, ‘now.’”
The post When Are the Best Years of Our Lives? appeared first on Specialdocs Consultants.
by Ivan | Sep 4, 2019 | Healthy Aging, Medical Conditions, Patient News
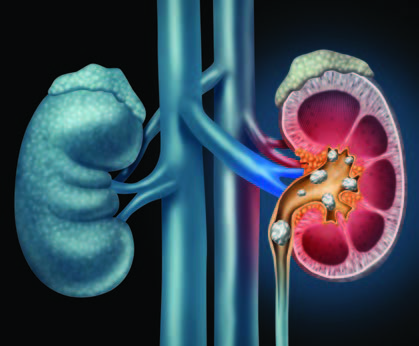
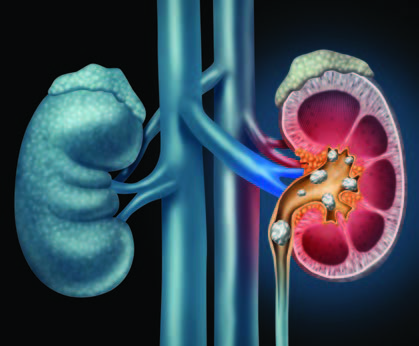
This Too Shall Pass: Treating and Preventing Kidney Stones
More common, frequently less painful and far more preventable than reputed, kidney stones have, entered a new era of highly effective, noninvasive procedures. We bring you up to date on kidney stone treatment & prevention
Q: Why do kidney stones happen?
A: They form when substances such as calcium, oxalate, cystine or uric acid are present at high levels in urine, becoming crystals that gradually increase in size to a stone. According to the Urology Care Foundation, Calcium stones are the most common (80%), with Uric Acid and Struvite / Infection stones making up the other 20%.
Q: How likely am I to experience kidney stones?
A: One in 10 people deal with kidney stones in their lifetime, more frequently men, but in recent years, women are rapidly closing the gap. Genetic factors also play a role: if kidney stones are prevalent among your family members, you are at higher risk of developing them.
Q: Are kidney stones very painful?
A: Over the years, the pain associated with kidney stones has taken on an almost mystical aura, sometimes described as “worse than childbirth.” However, the truth is that not every kidney stone causes intense pain. Some are small enough to pass unnoticed, and many are asymptomatic and only discovered when blood is found in the urine during routine testing. Others are large but can stay in the kidney forever without incident. It is only the stones that become “stuck” on their way out of the body that cause renal colic, or waves of severe pain, which can be promptly treated with pain medication.
Q: Does back pain mean I have kidney stones?
A: This is frequently asked by patients concerned about pain felt in the flank area near the kidney. A careful history will be taken to help determine the location of the pain, but a fairly simple way to distinguish the cause is to change positions. If the pain worsens, it is more likely to be a musculoskeletal type of strain. Kidney stone pain is less likely to be positional.
Q: How do you determine if treatment is needed?
A: A noninvasive, less expensive ultrasound is used for screening, but a spiral computed tomography (CT) scan provides superior imagery used to more accurately pinpoint the stone’s location. If only a partial obstruction is seen and not much pain is involved, time is on your side and we can wait to see if the stone passes naturally. At that point, many patients can rest comfortably at home and may be given antispasmodics (such as Flomax) to relax the ureter, pain medications to manage pain and instructed to drink plenty of water to aid the stone’s passage.
Q: What if it doesn’t pass on its own?
A: It’s reassuring to realize there is no urgency to remove the stone unless the kidney is obstructed or infected or the patient is experiencing intractable pain. And when removal is indicated, urologists (specialists in diseases of the urinary tract) have a number of options available, many of them noninvasive or minimally invasive. Open surgical procedures are a rare event. Instead, an outpatient ureteroscopy can be done, using an endoscope to break up or remove the stone. Even less invasive is lithotripsy, good for small stones, which directs high-energy shock waves toward the stone and breaks it into fragments to more easily pass out of the body. For extremely large or resistant stones, a minimally invasive percutaneous nephrolithotomy is conducted to remove the stone via an endoscope inserted through a small incision in the skin.
Q: What is the best way to prevent kidney stones from forming again?
A: We can take the time to develop an individualized approach, based on your stone’s composition. First, your stone will be tested and categorized as calcium oxalate (the most common type), calcium phosphate, a mix or a non-calcium type. Also recommended is a 24-hour urine collection to form a clear picture of how the crystals form in your body, as well as blood tests for further analysis. While those who have formed stones before are at higher risk for forming a subsequent one, we know that dietary modifications tailored to stone type and – if needed – drug therapy can substantially reduce that risk. If you form calcium oxalate stones, we’ll work on a plan to avoid foods high in oxalate, such as spinach, beets and rhubarb, and keep sodium consumption at a minimum. Also important to know is that despite its role in the stone’s composition, there is no need to restrict calcium. In fact, increasing your calcium intake with higher-calcium foods such as milk, yogurt and cheese can help lower oxalate levels in the urine. Finally, keep in mind that the single best preventive measure is to simply fill a bottle with water and drink often.
The post Kidney Stones: Treatment & Prevention appeared first on Specialdocs Consultants.







Recent Comments