by Ivan | Nov 26, 2019 | Healthy Aging, Patient News, Wellness

Life’s Happiness Continuum
Is there a predetermined peak age for happiness, before which our normal outlook is gloomy and melancholy and after which we slump back into these non-euphoric ways? When Are the Best Years of Our Lives?
Studies Show Two Stages of Life Happiness
Like trying to define why some people are born to be joyful and others to play the role of curmudgeon, this issue has long intrigued psychological and social science researchers. While no singular conclusion has been reached, there are a number of compelling hypotheses…and you may be pleasantly surprised to learn that a number of studies suggest a U-shaped happiness curve with peaks for young and old, giving us not one but two stages of life to savor. Mid-life can be stressful, full of the challenges and demands of raising a family and sustaining a career, but according to some experts, there is indeed a light at the end of the tunnel.
The Economist’s international survey of happiness gathered data from America’s General Social Survey, Eurobarometer and Gallup finding an upward trajectory of happiness until age 30, a downward trend into midlife, with the lowest point reached at age 46, and up to higher levels again after the 50’s. Jonathan Rauch, a senior fellow at the Brookings Institution and author of the 2018 book, The Happiness Curve, says although its effects vary between individuals, there appears to be a subtle but insistent tug that makes happiness more difficult to achieve in midlife and then reverses direction when we least expect it.
Other research supports this finding, including a University of Chicago retrospective study of 28,000 Americans over a 32-year period which showed older age groups were consistently the happiest. Interestingly, Dr. Dilip Jeste, director of the UC San Diego Center for Healthy Aging, describes it not as a curve, but more of a linear improvement in mental health that occurs even as physical and cognitive function declines.
Might Happiness in Women Peak Between the Ages of 50-70?
In particular, today’s women may find some of their sweetest times between ages 50 and 70, according to an in-depth lifestyle study spanning three decades conducted by the TrendSight Group. The take-away for younger generations: “Aging isn’t a dirty word, with it can come incredible confidence, strength and freedom,” says study author Marti Barletta. Even better, a full 59% of women ages 50 to 70 felt their greatest achievements were still ahead of them.
Happiness may Increase with Age
Experts theorize a number of reasons that happiness may increase with age, including increased wisdom or psychological intelligence in handling challenges, fewer aspirations and expectations of self, greater appreciation for life, living in the moment with less worry about the future, greater ability to regulate emotions and less worry about pleasing everyone all the time. Stanford psychologist Laura Carstensen’s Socioemotional Selectivity Theory, which is grounded in the unique human ability to monitor time, suggests that relative to younger people, older adults focus more on positive than negative information and prioritize emotionally meaningful activities – notably, deepening close relationships – over those related to individual achievement and exploration.
Recent findings from the Harvard Study of Adult Development, one of the world’s longest studies of adult life, begun in 1938, also point to the vital role of relationships in happiness at older ages. According to the research, these ties protect people from life’s discontents, help to delay mental and physical decline, and are better predictors of long and happy lives than social class, IQ or genes. Dr. Robert Waldinger, study director and psychiatrist at Massachusetts General Hospital, acknowledges that the research shows correlation, not necessarily causation. However, after following the subjects (including both Harvard graduates and inner-city residents) for many decades and comparing the state of their health and their relationships early on, he is confident that strong social bonds play a causal role in long-term well-being.
Perhaps 19th century journalist David Grayson had the best advice of all: “The other day a man asked me what I thought was the best time of life. ‘Why,’ I answered without a thought, ‘now.’”
The post When Are the Best Years of Our Lives? appeared first on Specialdocs Consultants.
by Ivan | Nov 26, 2019 | Medications, Patient News

Managing Prescription Drugs: From Pickup to Take Back
If you are not taking your prescription medications as directed (or at all), you’re far from alone. Compliance is estimated at just 50% among U.S. patients. Unfortunately, adherence is a direct impact on quality and length of life, and overall healthcare costs, accounting for up to 50% of treatment failures and up to 25% of hospitalizations each year. The reasons for noncompliance vary, from patients not being convinced of the medication’s effectiveness, fear of side effects, the cost of certain medications to difficulty using tools (such as inhalers) or an aversion to injections. What can be done to manage prescription drugs more effectively?
For most, non-compliance is simply an unintentional consequence of forgetfulness or lack of organization. When faced with the need to keep track of a growing lineup of daily doses – and 77% of older adults manage two or more chronic conditions according to the National Council on Aging – it can become challenging to keep up. Fortunately, many solutions are available, from old school pen and paper to high-tech smartphone apps, that make it easy to reap the benefits of and manage your prescription medications.
Pick up
- At the pharmacy, check your prescription instructions and make sure you fully understand dosage and timing; if best taken with food; interactions with other drugs, supplements, foods and alcohol; and side effects. If you have questions, ask the pharmacist or call our office.
Organize
- Tried and true, a pill organizer with compartments divided into sections for days of the week is most helpful in managing multiple medications. Keep the original bottles so you can quickly access any dosing and refill information printed on the bottle or packaging.
- Create a dosing schedule chart to keep next to the pill organizer, with a physical description or visual image of each pill. Use a spreadsheet or word processing program to make a list of all medications, times to take, and a check off space to indicate when taken. A number of pre-formatted charts are available online for download from the American Heart Association, the Food and Drug Administration and others.
- Online pharmacies are entering the mix, offering delivery of monthly medications sorted by dose.
Smartphone Reminders
Free smartphone apps can serve multiple functions. A few of the best:
- Medisafe medication management and pill reminder, highly rated by pharmacists for its comprehensiveness and usability, includes videos for many frequently used medications illustrating use, side effects, contraindications and other information, and emails you a history of your medications and doses in an Excel spreadsheet.
- Care Zone Health Information Organizer enables you to take pictures of your prescription and over-the-counter (OTC) drugs and supplements, populates with details, and sends reminders to take medications and refill prescriptions.
- Drugs.com also sends reminders, keeps your medication history, includes an interaction checker for other drugs and foods and provides access to updated information for more than 24,000 prescription and OTC drugs and supplements.
- Ask your pharmacist about preparing blister packs for daily or weekly medications; timer caps for pill bottles that beep to remind you when to take medications; gadgets that “talk” and relay the information verbally; and stand-alone electronic pill devices enabling easy input of medication name and measures, with an alarm that notifies you when the next dose is needed.
Properly Store your Prescription Drugs
- Pick a location that is up and away, like a kitchen cabinet (not the bathroom, unless it is well ventilated). Keep medications cool and dry and in a well-lit area to ensure you’ll reach for the right ones.
- Open the medicine bottle on a flat surface to prevent dropped pills from being lost down a drain or landing on the floor.
- Make a discard pile of medicines that are discolored, dried out, crumbling, leftover from a previous illness or past their expiration date—particularly biologic products, insulin, refrigerated liquids, eye drops, injectables or specially compounded medications.
Discard with care: Toss, flush or Take Back
Most prescription and OTC medicines can be thrown away in the household trash, with these important procedures:
- Do not crush tablets or capsules.
- Mix the medicines with kitty litter or used coffee grounds to prevent thievery or diversion of medicines from the trash. Then, place the mixture in a container such as a sealable plastic bag, and throw away.
- Remove the label and/or scratch off all personal information when disposing of a prescription vial.
- Check instructions included with prescription drugs such as narcotic pain relievers e.g. the fentanyl patch and other controlled substances, which must be flushed instead of discarded.
Even more convenient and environmentally sound are programs such as National Prescription Drug Take Back Day, sponsored by the U.S. Drug Enforcement Administration (DEA) in communities nationwide. The next one is scheduled for October 26, 2019: Find a collection site near you at https://takebackday.dea.gov, dispose of your unused or expired drugs safely and easily.
Did You Know?
Approximately 50% of medications for chronic disease are not taken as prescribed.
*Source: Annals of Internal Medicine
11.8 million pounds of prescription drugs collected since Take Back Day began in 2010.
*Source: Drug Enforcement Administration
The post Manage Prescription Drugs Effectively appeared first on Specialdocs Consultants.
by Ivan | Sep 4, 2019 | Healthy Aging, Medical Conditions, Patient News
This Too Shall Pass: Treating and Preventing Kidney Stones
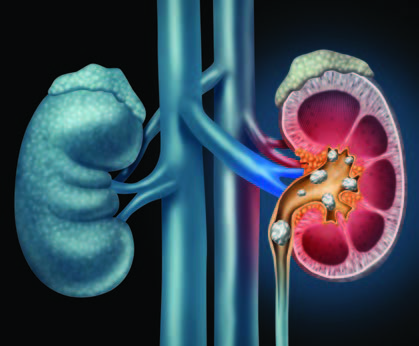
More common, frequently less painful and far more preventable than reputed, kidney stones have, entered a new era of highly effective, noninvasive procedures. We bring you up to date on kidney stone treatment & prevention
Q: Why do kidney stones happen?
A: They form when substances such as calcium, oxalate, cystine or uric acid are present at high levels in urine, becoming crystals that gradually increase in size to a stone. According to the Urology Care Foundation, Calcium stones are the most common (80%), with Uric Acid and Struvite / Infection stones making up the other 20%.
Q: How likely am I to experience kidney stones?
A: One in 10 people deal with kidney stones in their lifetime, more frequently men, but in recent years, women are rapidly closing the gap. Genetic factors also play a role: if kidney stones are prevalent among your family members, you are at higher risk of developing them.
Q: Are kidney stones very painful?
A: Over the years, the pain associated with kidney stones has taken on an almost mystical aura, sometimes described as “worse than childbirth.” However, the truth is that not every kidney stone causes intense pain. Some are small enough to pass unnoticed, and many are asymptomatic and only discovered when blood is found in the urine during routine testing. Others are large but can stay in the kidney forever without incident. It is only the stones that become “stuck” on their way out of the body that cause renal colic, or waves of severe pain, which can be promptly treated with pain medication.
Q: Does back pain mean I have kidney stones?
A: This is frequently asked by patients concerned about pain felt in the flank area near the kidney. A careful history will be taken to help determine the location of the pain, but a fairly simple way to distinguish the cause is to change positions. If the pain worsens, it is more likely to be a musculoskeletal type of strain. Kidney stone pain is less likely to be positional.
Q: How do you determine if treatment is needed?
A: A noninvasive, less expensive ultrasound is used for screening, but a spiral computed tomography (CT) scan provides superior imagery used to more accurately pinpoint the stone’s location. If only a partial obstruction is seen and not much pain is involved, time is on your side and we can wait to see if the stone passes naturally. At that point, many patients can rest comfortably at home and may be given antispasmodics (such as Flomax) to relax the ureter, pain medications to manage pain and instructed to drink plenty of water to aid the stone’s passage.
Q: What if it doesn’t pass on its own?
A: It’s reassuring to realize there is no urgency to remove the stone unless the kidney is obstructed or infected or the patient is experiencing intractable pain. And when removal is indicated, urologists (specialists in diseases of the urinary tract) have a number of options available, many of them noninvasive or minimally invasive. Open surgical procedures are a rare event. Instead, an outpatient ureteroscopy can be done, using an endoscope to break up or remove the stone. Even less invasive is lithotripsy, good for small stones, which directs high-energy shock waves toward the stone and breaks it into fragments to more easily pass out of the body. For extremely large or resistant stones, a minimally invasive percutaneous nephrolithotomy is conducted to remove the stone via an endoscope inserted through a small incision in the skin.
Q: What is the best way to prevent kidney stones from forming again?
A: We can take the time to develop an individualized approach, based on your stone’s composition. First, your stone will be tested and categorized as calcium oxalate (the most common type), calcium phosphate, a mix or a non-calcium type. Also recommended is a 24-hour urine collection to form a clear picture of how the crystals form in your body, as well as blood tests for further analysis. While those who have formed stones before are at higher risk for forming a subsequent one, we know that dietary modifications tailored to stone type and – if needed – drug therapy can substantially reduce that risk. If you form calcium oxalate stones, we’ll work on a plan to avoid foods high in oxalate, such as spinach, beets and rhubarb, and keep sodium consumption at a minimum. Also important to know is that despite its role in the stone’s composition, there is no need to restrict calcium. In fact, increasing your calcium intake with higher-calcium foods such as milk, yogurt and cheese can help lower oxalate levels in the urine. Finally, keep in mind that the single best preventive measure is to simply fill a bottle with water and drink often.
The post Kidney Stones: Treatment & Prevention appeared first on Specialdocs Consultants.
by Ivan | Aug 1, 2019 | Nutrition, Patient News

Considering Keto: Is It the Right Diet for You?
The truth is that a silver bullet for weight loss likely does not exist, but Americans’ perpetual search continues unabated. Low-carb diets such as Paleo, Whole30, and most prominently, Ketogenics, or “keto” may be the latest contenders, yet Academy of Nutrition and Dietetics spokesperson Ginger Hultin, RD, reveals she’s never seen a more popular – or more misunderstood – trend, the Keto Diet…..
Keto’s guidelines dramatically change typical eating patterns, with an emphasis on high fats (accounting for 80% of daily calories); moderate proteins (10 to 20% of daily calories); restricted carbs (5 to 10% of daily calories – ideally 20 to 30 grams a day, or the equivalent of a medium apple); and elimination of all grains, starchy vegetables and high-carb fruits. This means a diet replete with meats, butter, seeds, avocado and oily fish, but little or no bread, potatoes, corn, beans, legumes, milk, beer, sugar or fruits like bananas and pears.
The concept, according to Hultin, is that getting most of your calories from fat forces the body to enter ketosis and burn stored fats. Here’s how: In the absence of circulating blood sugar, which comes from carbohydrates, the body starts breaking down stored fat into molecules called ketones via a process called ketosis. Once ketosis is reached, usually within three to four days of eating less than 20 to 50 grams of carbohydrates daily, ketones are used to generate energy in the body until carbohydrates are eaten again.
Earlier research showed ketosis has benefits for blood sugar control among people with diabetes, and its efficacy has been proven in controlling seizures in some patients with epilepsy. Most people are attracted to keto based on the promise of shedding pounds quickly, which is when the diet’s drawbacks become glaringly evident.
“When followed consistently for the short term, the keto diet can lead to rapid weight loss,” says Hultin. “However, when people stop following it, as is inevitable on a highly restrictive diet, the weight is just as quickly regained, plus more.”
Side effects of a keto diet range from constipation due to lack of fiber to a potential negative impact on liver and kidney function, and limiting vitamin- and mineral-rich fruits, vegetables and grains is a concern for sustaining heart health. Hultin believes keto’s limited choices can also be socially isolating to dieters.
“The keto diet may be a quick fix but is not a sustainable solution,” she says.
There is no debate around the life-changing aspects of the keto diet for young patients with epilepsy, but experts agree that the long-term effects on others warrant further research before recommendations can be made. For those still interested in trying keto, a focus on healthier fats is essential, rather than options such as bacon and cheese. Additionally, be sure to test and monitor your blood cholesterol levels, as studies show many keto dieters experience an unwanted increase in these numbers.
Other trendy diets may fare no better in terms of sustainability. Whole30 takes a deliberately short-term approach with a 30-day plan that eliminates all sugar, alcohol, grains, legumes and dairy and focuses on moderate amounts of meat, seafood and eggs; plenty of vegetables; some fruit; and natural fats. Most people return to their previous eating habits after the monthlong experiment, according to Mayo Clinic. A paleo diet focuses on foods that were hunted and gathered during the Paleolithic era, and typically includes lean meats, fruits, vegetables and nuts, but eliminates whole grains, legumes and dairy products, making it challenging to adopt long-term.
The ideal diet? One that places the greatest emphasis on nature’s bounty of fruits and vegetables; encourages whole foods, whole grains, healthy oils, moderate amounts of protein, and does not eliminate entire categories of food.
“Find a diet that’s flexible enough to let you feel good about your relationship with food … and enjoy your life!” advises Hultin.
Did You Know?
Because fasting can put a person into ketosis, intermittent fasting can also be considered a type of ketogenic diet.
The post Keto Diet: Right for You? appeared first on Specialdocs Consultants.
by Ivan | Jul 9, 2019 | Patient News, Staying Active, Wellness

Wake-up Call: Fighting Fatigue at Its Roots
Feel like you are fighting fatigue throughout the day, the joy in life slowly diminishing and your active lifestyle becoming a distant memory? Are these ordinary signs of aging?
No, no and no!
Feeling tired all the time is not a normal part of the aging process. Instead, it can point to the need for a better night’s sleep, stress or an underlying illness, or be the result of a mix of common medications. Or it may be a combination of all these things. Identifying the possible sources of your fatigue is the most important step in reenergizing your lifestyle.
Medical: Visit your physician to rule out these frequently seen causes of tiredness.
Emotional health: Low-grade depression, anxiety or chronic stress can sap energy.
Anemia: This condition occurs when your blood has too few red blood cells or those cells have too little hemoglobin, a protein that transports oxygen through the bloodstream. If untreated, anemia results in a drop in energy levels.
Heart disease: When the heart pumps blood less efficiently, it can lead to fluid in the lungs, causing shortness of breath and reducing the oxygen supply to heart and lungs.
Hypothyroidism : An underactive thyroid gland can cause fatigue – along with other symptoms, such as weight gain, weakness, dry skin, feeling cold and constipation.
Medications : Many medicines can cause fatigue, including blood pressure drugs, antidepressants, anti-anxiety drugs and antihistamines.
Lifestyle Habits
Sleep: Quality, quantity and environment matter greatly in ensuring a healthy sleep, but these factors are surprisingly misconstrued. According to NYU School of Medicine, dispelling these widely held beliefs is key:
- Myth: “Alcohol before bed is good for sleeping.” A nightcap before bed may help you fall asleep but will dramatically reduce the quality of sleep by disrupting the REM (rapid eye movement) stage all night, and you’ll wake unrefreshed.
- Myth: “Many adults need only five hours of sleep or less, especially as they get older.” The reality is everyone needs to get enough sleep to wake up feeling refreshed. The average is seven to eight hours nightly to allow the body to progress through four phases of restorative sleep, including deep sleep cycles of REM and delta waves sleep, which are important for generating neurons, repairing muscle and restoring the immune system.
- Myth: “Watching TV in bed before sleep is a good way to relax.” Actually, turning off the TV and putting away electronic devices at least two hours before bedtime is recommended, as the blue light produced affects the release of melatonin, the sleep hormone, and will delay slumber.
- Myth: “If I wake up in the middle of the night, it is best to lie in bed until I fall back asleep.” Tossing and turning for more than 20 minutes is not helpful; instead, change rooms and engage in something mindless, like folding socks. Do not watch TV or look at electronic devices, as this wakes up your brain.
- Myth: “Snoring is a common, harmless problem.” Snoring can be a sign of sleep apnea, a disorder characterized by decreased or complete lack of airflow throughout the night. Over time, this can increase the risk of cardiovascular disease if untreated.
- Myth: “Falling asleep anywhere, anytime is the sign of a good sleeper.” It’s just the opposite, indicating a sleep “debt” from insufficient rest or a sleep disorder such as narcolepsy or sleep apnea.
Under- or over-activity: Sedentary days and nights can cause loss of muscle mass and flexibility and make even moderately intense activities seem exhausting. However, exercising at a very high intensity can also cause fatigue.
An Infusion of Energy for Chronic Fatigue Research

Far beyond ordinary tiredness is the profound fatigue known as myalgic encephalomyelitis/ chronic fatigue syndrome (ME/CFS), which has puzzled and frustrated medical professionals for decades. No cure or approved treatment is available to its 2.5 million sufferers, only a management of symptoms worsened by any type of physical, cognitive or emotional effort. But a sea change is underway. It began in 2015 with a new name recommendation by the Institute of Medicine (IOM): Systemic Exertion Intolerance Disease (SEID). Noting that the term chronic fatigue syndrome can trivialize the seriousness of the condition and that “ME” is inappropriate because neither muscle pain nor brain inflammation has proven to be a symptom, the IOM panel stated: “SEID captures a central characteristic of this disease – that exertion of any sort can adversely affect patients in many organ systems and in many aspects of their lives.”
Even more promising is the significant investment in research announced by the National Institutes of Health (NIH). Up to $36 million over five years has been granted to shine a brighter light on the origins and progression of chronic fatigue and ultimately to help develop diagnostic markers and effective treatments for fighting fatigue.
Did You Know?
58% of older adults sleep less than seven hours a night.
80% of people age 55 and over report unintentionally falling asleep at least once during the day within the last month.
Source: Centers for Disease Control and Prevention
The post Fighting Fatigue appeared first on Specialdocs Consultants.
by Ivan | Apr 2, 2019 | Healthy Aging, Patient News, Staying Active
Ramping Up your Sprint Fitness after a Long, Sedentary Winter
Whether you went into hibernation as the result of a record cold winter season, or took time off from your usual exercise routine because of a busy schedule or illness, spring is an ideal time to get back in action. When done with care, starting or rebooting your fitness regimen this spring will set you up for a vibrant, energetic summer. After being cleared for exercise by our office, consider these issues to ensure you’re not sidelined by injury, fatigue or boredom and get the most out of your spring fitness efforts
Aerobic or strengthening exercise?
Both. According to the 2018 Physical Activity Guidelines for Americans, any amount is helpful but the recommendations to help prevent chronic diseases is 150 minutes of moderate-intensity or 75 minutes of vigorous-intensity, aerobic activity is recommended each week, and muscle-strengthening activities (free weights or resistance bands) two or more days a week. It would be ideal for older adults to add balance training to the mix. If it’s challenging to find long periods of time to exercise, note that three 10-minute bouts or one 30-minute bout will deliver equal improvements in fitness.
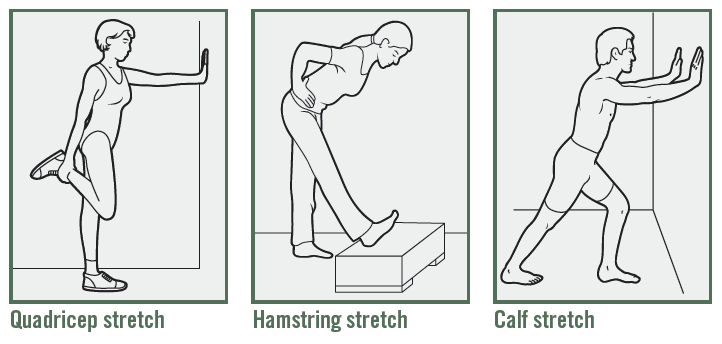
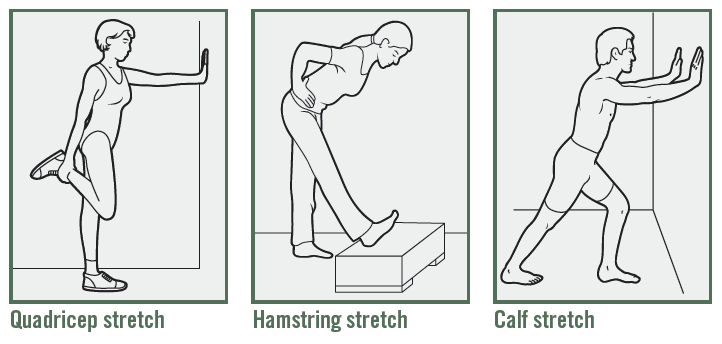
Stretch before or after exercise?
Before, after or both can all work well, if done properly. Do not attempt long stretches beforehand when your muscles are cold and you’re likely to pull a tendon, cautions Christine Butz, Doctor of Physical Therapy at Athletico. Instead, take 10 minutes to pedal on a stationary bike, march in place or walk around. Post exercise is the time for long, 30-second stretches that help you slowly increase muscle length (see below for examples). Most importantly, don’t push through pain, says Butz. “If you experience sharp, persistent pain, or have difficulty moving through a full range of motion, stop and see a physician to determine if it’s a strain, tear or fracture.”
Steady state or interval training?
Once the bastion of elite athletes, interval training can be used at any level, according to Mayo Clinic. Simply alternate short bursts (approximately 30 seconds) of intense activity with longer intervals (three to four minutes) of less intense activity. For instance, if your exercise is walking, try incorporating a brief surge of jogging into your regular walks or alternate leisurely strolling with periods of brisker walking. As your cardiovascular fitness improves, you’ll be able to exercise longer or with more intensity during your spring fitness routine.
What are the best activities to try?
Tap into one of these fitness trends to reinvigorate your workouts:
- Starting with Jazzercise in the 1980s, and rising again in the 2000s with Zumba, both of which remain popular, numerous dance-centric classes are offered at health clubs and park districts – Broadway show routines, tap dancing, belly dancing, Irish dancing, square dancing, line dancing and ballet-inspired barre workouts. Interesting note: a number of studies are in progress exploring the possible benefits of dance in enhancing cognitive function and reducing stress.
- Indoor cycling classes such as SoulCycle, Flywheel and CYC provide a fast-paced, high-energy environment. If you prefer to stay outdoors, but feel a bit unsteady on a 10-speed racer, check out the proliferation of classic cruiser bikes featuring wide, comfortable seats and upright handlebars.
- Yoga and Pilates. Both are low-impact workouts that focus on using bodyweight resistance. Yoga builds strength, balance (ideal for preventing falls) and harmony in mind and body, with breathing exercises, meditation and postures (asana or poses) that stretch and flex various muscle groups. Pilates is excellent for improving core strength and recovering after injury.
- Water classes are another low-impact option to build core muscles and help improve flexibility, stability and balance. Choices include traditional aqua aerobics as well as aqua ballet, aqua yoga and aqua tai chi.
- Functional Training classes are designed to improve balance, coordination, agility, speed and strength, such as BOSU (both sides utilized) ball workouts.
The post Spring Fitness appeared first on Specialdocs Consultants.






Recent Comments