
by Specialdocs Consultants | Jul 11, 2023 | Patient News, Wellness
Summertime is prime time for ticks, which are becoming more prevalent each year. A combination of changing land use and warmer winters has greatly expanded the ticks’ habitat and they’re now found in more than half of U.S. counties. As a result, tick-borne Lyme disease has doubled over the last two decades to nearly 500,000 cases annually, earning it the unfortunate distinction of being the most common vector-borne illness in the Northern hemisphere. Read on for details on how to protect yourself this season, and in the summers to come.
Identifying Lyme
In its acute phase (one to two weeks after the bite), Lyme can cause fevers and chills, joint pain, headache, muscle aches and is frequently accompanied by a salmon-colored rash at the site of the tick bite. It may have a “bulls-eye” appearance, often considered a sign of infection, but the rash can manifest differently, or not at all. Diagnosis is based on symptoms, physical findings (e.g., rash), the possibility of exposure to infected ticks, and antibody tests. A high number of false negative tests occur in the early phase, however, because it takes time for the immune system to respond to the infection and create antibodies. As the infection progresses, virtually everyone with Lyme disease has a positive test result.
Treating early, late and long Lyme
Most people recover from Lyme disease rapidly and completely if diagnosed early and treated with a short course of oral antibiotics. More serious symptoms, including joint pain and swelling, nerve problems and neurological issues, may develop if Lyme disease is left untreated. Known as late Lyme disease, it can occur months to years after a tick bite, and requires a longer course of antibiotics, administered intravenously. Post-Treatment Lyme disease, sometimes called chronic or long Lyme disease, is experienced by 5% to 15% of patients who have lingering symptoms such as headache, fatigue, joint pain and “brain fog.” While the condition is not yet well understood, experts have found additional antibiotic treatments are not usually helpful, and the symptoms gradually resolve over time.
Preventing Lyme
The best way to avert the complications of Lyme disease is to vigilantly avoid ticks. These tips can help you prevent Lyme disease:
- Wear shoes, long pants tucked into socks, a long-sleeved shirt, hat and gloves in wooded or grassy areas.
- Stick to trails, stay clear of low bushes and long grass.
- Use insect repellants such as DEET, picardin, permethrin (apply to clothing).
- Do tick checks on your body after outside activities. Be sure to check your dogs for ticks
too!
- Remove any ticks promptly with clean, fine-tipped tweezers. Be reassured that just finding a tick on your skin doesn’t mean you’ll get Lyme disease; a tick needs to be attached for at least 48 hours before it can transmit the bacteria.
- Look for advanced protection in the next few years from two well-known names in vaccines – Pfizer and Moderna. An earlier vaccine, LYMERix, was discontinued in 2002 due to lack of interest at a time of lower Lyme disease cases, as well as concerns over side effects. Pfizer’s VLA15 is intended to block the bacteria from leaving the tick. Moderna is applying mRNA technology used in its COVID vaccine to target the Borrelia bacteria species at the root of most U.S. Lyme disease cases. Also of note is MassBiologics’ shot that delivers a single, human anti-Lyme antibody directly to a person to provide immediate immunity…now in trials.
QUICK BITES: Fast Facts About Lyme Disease
- Most Lyme disease infections in the U.S. occur May through September.
- Cases of Lyme disease are most commonly seen in the northeast and mid-Atlantic states
(from Maine to Virginia), the Midwest (Minnesota, Wisconsin, and Michigan), and the
West Coast (California).
- The disease was first recognized in Old Lyme, Connecticut in 1975 when a cluster of
children developed unexplained, rheumatoid arthritis-like symptoms. Not until the next decade was the cause discovered: the spiral bacteria Borrelia burdorferi in deer ticks prevalent in the forests near where the infections occurred. Testing confirmed the Lyme disease bacterium was passed to humans via the bite of a deer tick.
Sources: NIH, National Geographic

by Specialdocs Consultants | Oct 6, 2022 | Healthy Aging, Patient News, Wellness
Senior Moments Or Something More?
As Baby Boomers continue the inexorable journey deep into their senior years, preserving cognitive function understandably tops the list of worries. While Alzheimer’s Disease and related dementias are seen in just 5% of people over 65, that number jumps to 30% for people age 85 and over. Questions abound: is forgetting a name a sign of normal aging or an indicator of a more serious memory disorder? Are any nutritional supplements or pharmaceutical treatments available that are proven to stave off memory loss? Most importantly, what steps can be taken to modify individual risk?
To better understand how to identify and manage dementia and Alzheimer’s disease, we asked one of the country’s leading experts, R. Sean Morrison, MD, for his informed perspective on this growing concern for seniors, their families and caregivers. A practicing geriatrician, palliative medicine physician and health researcher for almost three decades, Dr. Morrison has earned numerous awards and recognition for his work, and currently serves as the Chair of the Brookdale Department of Geriatrics and Palliative Medicine at the Icahn School of Medicine at Mount Sinai and as Director of the Hertzberg Palliative Care Institute.
 Is memory loss an inevitable, natural sign of aging?
Is memory loss an inevitable, natural sign of aging?
Dr. Morrison: The good news is that not all cognitive functions decline with age. The ability to maintain attention, language comprehension, usage, and vocabulary does not decrease. Knowledge learned years ago like how to ride a bike, or brush your teeth, also stays intact. Additionally, when you learn something new and can remember it, you won’t forget it any more rapidly than when you were younger.
The not so good news is that it will take greater effort to learn those new things; more attention, repetition and use of memory-enhancing strategies will be needed. The ability to multitask is also diminished, as processing information takes longer and reaction times are slower. People may experience poorer performance when working under time pressure, and find it more difficult to manipulate information in the brain, such as calculating a tip in a restaurant or figuring out a route to travel from one place to another.
 How do you distinguish between a “senior moment” lapse in memory and a sign of Alzheimer’s disease?
How do you distinguish between a “senior moment” lapse in memory and a sign of Alzheimer’s disease?
Dr. Morrison: So many people experience that temporary inability to remember a name. But if you are able to recall things with a cue or can pick it out from a list of possibilities, that’s evidence of a problem with retrieval but not with storage. You can be reassured that it doesn’t indicate Alzheimer’s disease but a “senior moment” because the information has been successfully stored in your memory.
 Is routine screening for dementia recommended in older adults?
Is routine screening for dementia recommended in older adults?
Dr. Morrison: The U.S. Preventive Services Task Force does not recommend for or against routine screening, saying no interventions are proven to have a significant effect in people with earlier detected cognitive impairment. However, it is required as part of Medicare’s yearly assessments, and most primary care physicians consider dementia screenings an essential part of their annual wellness exam.
 What types of screening tests do you recommend?
What types of screening tests do you recommend?
Dr. Morrison: At least a dozen tests are available, each with their own benefits and drawbacks. I recommend the following for their ease of use and proven sensitivity and specificity in diagnosing cognitive impairment:
- Mini-Cog is a quick, three-minute evaluation. Patients are asked to repeat three words, draw a clock with hands at a specific time, and then recall the initial three words.
- Memory Impairment Screen assesses free and cued word recall. Patients are read four unrelated words from four categories (e.g. Red Cross, saucer, checkers, telegram) and after a few minutes of diversion, asked to recall the words in 20 seconds, either with no prompting or cued by category.
- Animal Fluency Test. Patients are asked to name as many animals as possible in a 60-second period.
 Are there any risk factors for dementia and Alzheimer’s disease that can be controlled by patients?
Are there any risk factors for dementia and Alzheimer’s disease that can be controlled by patients?
Dr. Morrison: Quite a few risk factors are modifiable with lifestyle changes and non-pharmaceutical treatments. These include:
- Address hearing and visual impairments, with eyeglasses, hearing aids and other assistance
- Prevent and manage hypertension and diabetes
- Maintain a healthy weight
- Stop smoking
- Seek treatment for depression
- Prioritize regular exercise and physical activity
- Avoid social isolation
- Explore cognitive training
The best advice I can give to people in their 50s to 70s looking to prevent or delay progression of dementia and Alzheimer’s disease: exercise, exercise, exercise and rigorously control your blood pressure.
 How are the symptoms frequently experienced by people with dementia – sleep disturbance, mood disorders, agitation – best addressed?
How are the symptoms frequently experienced by people with dementia – sleep disturbance, mood disorders, agitation – best addressed?
Dr. Morrison: There are a number of non-pharmaceutical interventions that have proven effective. Use adaptive clothing and assistive devices to help eliminate distress around bathing and dressing. Create a reassuring familiar structure to the day with a regular routine and activities. Optimize the sleep environment with a comfortable temperature, the right amount of light, a warm milky drink and a bath or shower before bed; avoid stimulating medications, drinks containing caffeine and alcohol, and exercise too close to bedtime. Pharmaceutical treatments can also be considered, including antidepressants to improve cognition and ameliorate agitation and aggression, and melatonin and melatonin antagonists to help with sleep disorders. Of note: medications such as benzodiazepines (BZD), non-BZD hypnotics, mood stabilizers and antipsychotics are no longer routinely recommended as side effects can outweigh possible benefits.
 Are there any benefits to nutritional supplements or appetite stimulants?
Are there any benefits to nutritional supplements or appetite stimulants?
Dr. Morrison: Nutritional supplements can help with weight gain in patients with anorexia or cachexia (‘wasting’ syndrome) but have no meaningful impact on survival. And while appetite stimulants such as cannabinoids and steroids are often given to help patients with dementia, there is no consistent data regarding their safety and efficacy.
 What medications are available to treat or stop the progression of dementia?
What medications are available to treat or stop the progression of dementia?
Dr. Morrison: Until last year, only four medications were approved for treatment of dementia and Alzheimer’s disease, showing only a minimal to modest improvement in cognition. In 2021 a fifth drug was launched – aducanumab – a monoclonal antibody designed to reduce amyloid protein in the brain. Its fast-track approval was quite controversial as the clinical benefits of the drug were not proven during trials, which were stopped early as a result, and some severe side effects were observed. Interestingly, some researchers are now rethinking the idea that targeting amyloid protein plaques will eliminate Alzheimer’s disease, and instead exploring Alzheimer’s as a disease of inflammation. This could be the next fascinating line of research.
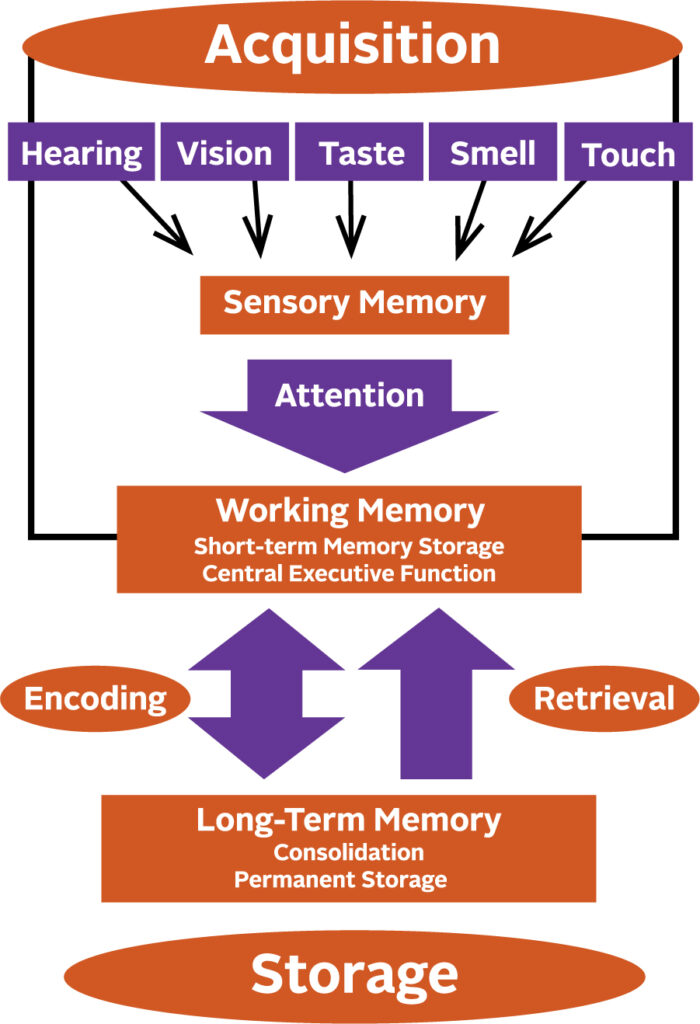
How a Memory is Made
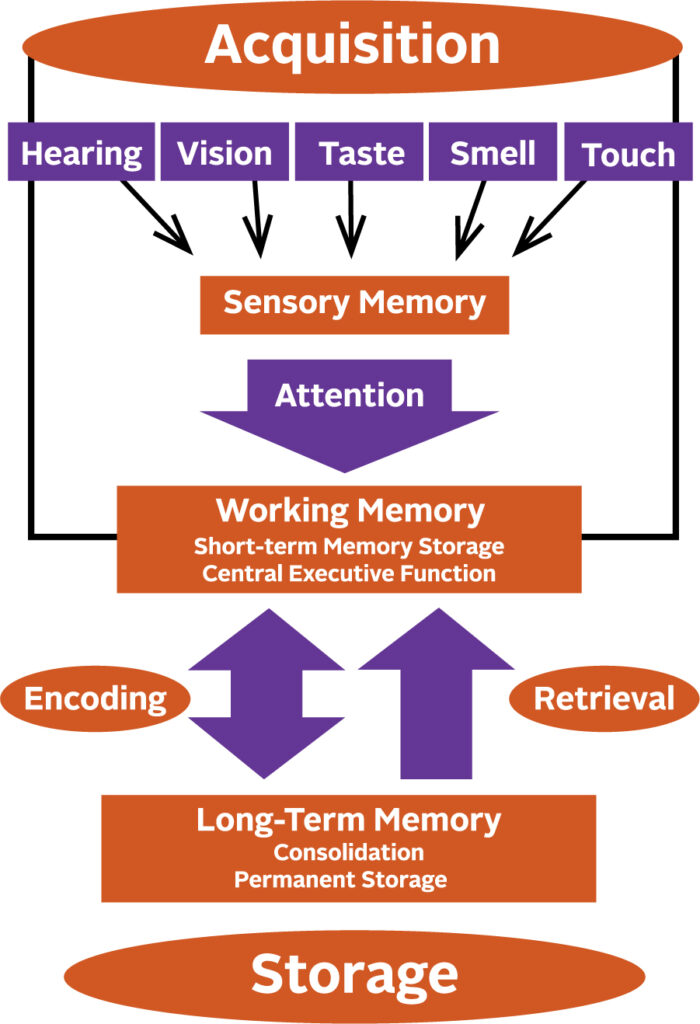
Memory begins to form by giving attention to the information received through your senses. Anything that interferes with your ability to pay attention, such as hearing impairment, will affect the formation of a sensory memory. Successful integration of sensory memories into your working memory enables you to temporarily store, organize and manipulate information. These memories are then encoded into long-term memory and finally put into permanent storage.

by Specialdocs Consultants | Jul 8, 2022 | Patient News, Wellness
Stay Safe with Sunscreen, Sunglasses and Plenty of Water
The longer, sunshine filled days of summer are upon us and without a doubt, they are one of life’s unrivaled joys, especially when you protect yourself from the powerful impact of ultraviolet rays. With that in mind, we share our tips for safe summer fun; from choosing and using the right sunscreen to staying hydrated.
The debate around sunscreen safety heated up with last year’s recall of some popular consumer products containing chemicals such as benzene, which is absorbed through the skin and into the bloodstream. Yet according to the FDA, the American Academy of Dermatology and other experts, there is minimal evidence that systemic absorption of these ingredients is toxic or harmful to health. There is, however, a mountain of proof regarding the harmful effects of sunburn – most notably its significant contribution to the risk of melanoma.
“Use of a broad-spectrum, SPF 30 sunscreen effectively blocks UVB and UVA rays to prevent sunburn,” says Dr. Andrea Murina, MD, associate professor of dermatology at Tulane University School of Medicine and director of the University Medical Center’s dermatology clinics. “This not only reduces the risk of developing skin cancer but also decreases signs of early aging on your skin (such as wrinkles, age spots, sagging skin) and stops existing melasma from darkening and new patches from appearing.”
According to Dr. Murina, while we know some ingredients in sunscreen do cross over into the bloodstream, most are rated by the FDA as GRASE, meaning generally recognized as safe and effective.
A bit of background: Earlier studies conducted by the FDA showed that common chemical ingredients used in sunscreen, including oxybenzone are absorbed into the bloodstream.
Further research on whether systemic absorption of oxybenzone was an actual concern was suggested. However, no clear links to any health problems in humans were identified.
Nevertheless, the ingredient has been eliminated from most sunscreens currently being manufactured, making it easy to find an oxybenzone-free product.
When applied correctly, a water-resistant, SPF 30 sunscreen is optimal, blocking 97% of UVB rays. “A higher SPF is fine, but only incrementally blocks more rays, and the time and duration of effectiveness is the same,” says Murina.
The best way to protect yourself is by using a combination of measures:
- Wear sun-protective clothing, including a lightweight, loose-fitting, long-sleeved shirt, pants, a wide-brimmed hat and sunglasses. Darker colors, densely woven cloth, unbleached cotton and shiny polyesters are recommended by the Skin Cancer Foundation.
- Judiciously apply broad-spectrum sunscreen every two hours on uncovered body parts, such as top of hands, face, neck and ears.
- Swap out regular SPF 15 foundation for a tinted sunscreen. “There are so many cosmetically elegant ones available today that mimic the look of makeup but offer much more protection,” says Murina. Tinted sunscreens with an SPF of 30 or higher provide protection that blends well with all types of natural skin tones, and help prevent exposure to both UV rays and visible light from the sun.
- Seek shade when the sun’s rays are strongest, between 10:00 a.m. and 2:00 p.m.
Like sunscreen, sunglasses are vital in blocking the harmful effects of UV radiation. UVA and UVB rays can cause increased risk of conditions such as cataracts, eye cancers and growths on the eye, as well as premature aging of the delicate skin around your eye. Choose sunglasses that block 99% or 100% of all UV light or are listed as having UV absorption up to 400nm. Wear them even when it’s hazy or cloudy, as UV light can pass right through clouds. And although you’ve undoubtedly heard this piece of advice before, it bears repeating: To protect your retina, never look directly at the sun.
Finally, drink up when you’re out in the sun. Water is the elixir of choice, helping to lower your body temperature and replace the fluids you lose through sweating. This is particularly important for older adults whose body’s fluid reserve becomes smaller and thirst sense decreases as they age. Be aware of the most common signs of dehydration – lightheadedness, fatigue, dizziness, less frequent urination, dark-colored urine – and rehydrate promptly with cool water.
Safe Travels
If your summer vacation includes international travel, we recommend some healthy pre-planning that includes the following:
- COVID-19: Make sure you are up to date with your vaccines and boosters. Get tested for COVID-19 as close to the time of your departure as possible (no more than three days before travel). Do not travel if you have COVID-19 symptoms, if you tested positive or if you are in quarantine due to possible exposure.
- Check the U.S. Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO) websites for the most up-to-date travel alerts, advisories and recommendations. Immunizations needed will vary based on your health condition, immunization history, countries and regions on your itinerary, and duration of your visit.
- Update your routine immunizations to protect against increased risk of exposure to illnesses such as seasonal flu, diphtheria, varicella (chickenpox), measles, mumps and rubella. For quick guidance on additional immunizations you may need, try the online tool at GlobalTravEpiNet.
- To protect yourself from the serious diseases spread by mosquitos, such as dengue fever and malaria, bring an EPA-registered insect repellent with an active ingredient like DEET or picaridin.
- Pack your prescription medications and consider bringing over-the-counter medicines, including anti-diarrheal medicine, antacid, antihistamine, hydrocortisone cream, motion sickness medicine, cough medicine, pain and fever medicine, and mild laxative.
- Also, pack supplies to prevent illness or injury, such as hand sanitizer, water purification tablets, insect repellent and sunscreen; and first aid items such as antibacterial ointment, antiseptic wound cleanser, aloe gel, insect bite cream, a digital thermometer and bandages.
We encourage you to contact your health care provider four to six weeks prior to your trip for personalized guidance … and we wish you a safe and memorable journey!
Sources: FDA, American Academy of Dermatology, Mayo Clinic, American Academy of Ophthalmology, U.S. Centers for Disease Control and Prevention, Skin Cancer Foundation

by Specialdocs Consultants | Apr 1, 2022 | Patient News, Staying Active, Wellness
Get Up and Join the Movement
As we emerge from the doldrums of winter hibernation and COVID-19-related inertia, it’s important to remember that exercise is good medicine and there’s no better time than now, to get moving again.
“There isn’t a chronic condition that can’t be better managed with an appropriate dose of exercise,” asserts Dr. Cedric Bryant*, President and Chief Science Officer at the American Council on Exercise. “This requires good interaction with your physician, an ability to listen smartly to your body and the realization that some exercise is always better than none.”
He recommends fostering good muscular fitness and enhancing strength, flexibility and balance with the exercise routine shown below. The 15-minute investment of time needed to complete one set of 8 to 15 repetitions for each exercise provides beginners with “the minimum effective dose needed to elicit a very positive response,” says Dr. Bryant.
Add regular rounds of exercise that build endurance, helping improve the health of your heart, lungs and circulatory system. To achieve the best results, you should have enough breath to talk but not enough to sing during aerobic activities such as brisk walking or jogging, dancing, biking, swimming, climbing stairs, or playing basketball, tennis or the uber-popular pickleball. (Learn more about today’s fastest-growing sport in an upcoming newsletter.) Be sure and check with your healthcare provider before beginning an exercise program.
Dr. Bryant’s Essential Seven
 1. Pushups
1. Pushups
Benefits: Develop the large muscles of the chest and the back of arms
The basic incline pushup is done using a sturdy table or other solid surface about 3 feet high. Stand facing the table and place your hands on the edge (shoulder width apart) arms straight and elbows not locked. Walk your feet backward until your arms and body are in a straight line. Bend elbows and slowly lower chest to the edge of the table while inhaling. Keep body straight and rigid throughout the movement. Push body away from the table until elbows are extended but not locked. Exhale as you push up.
 2. Bodyweight Squat
2. Bodyweight Squat
Benefits: Strengthens and tones the lower body
Stand with your feet slightly more than hip width apart, toes turned slightly outward, hands at sides with palms facing in. Pull shoulders down and back. Stiffen your core and abdominal muscles. Hold chest up and out, tilt head slightly up, shift weight back onto your heels while pushing hips toward the wall behind you.
Downward phase: Shift hips back then down to create a hinge-like movement at hips and knees. Try to control the amount of forward movement of the shinbones. Maintain tension in the core muscles and keep your back straight. Lower yourself until thighs are parallel or almost parallel with the floor. DO NOT go deep enough to cause pain. Make sure your feet don’t move, ankles don’t collapse in or out, knees remain aligned over the second toe, and body weight is evenly distributed between balls and heels of the feet.
Upward phase: Extend the hips and knees by pushing your feet into the floor. Hips and torso should rise together while heels are flat on floor and knees are aligned over the second toe. Continue extending until you reach the starting position.
Remember to inhale on the way down and exhale on the way back up.
 3. Bent-Over Row
3. Bent-Over Row
Benefits: Targets muscles in the upper and middle back and improves stability of the spine
Holding a small weight in each hand and standing with feet hip-distance apart, bend at the waist. Your back should be parallel to the floor with a neutral, not rounded, spine. Extend arms toward floor, keeping knees slightly bent. Engage abs and squeeze shoulder blades together as you bend elbows back and bring weights to your torso. Keep arms close to your torso. Slowly lower the weights back to the starting position.
 4. Modified Single-Leg Deadlift
4. Modified Single-Leg Deadlift
Benefits: Strengthens and tones gluteals and helps improve balance
Position yourself by a wall or chair. Stand straight, with feet aligned with hips, and shift weight to right leg. Slowly bend forward at the waist while raising your left leg behind you until your torso and leg are both parallel to the floor. Keep your head up and arms straight, perpendicular to the floor. Lower your leg as you return to an upright position. Keep your leg straight at all times. Repeat all reps on one side, then switch legs.
 5. Overhead Front Press
5. Overhead Front Press
Benefits: Increases shoulder strength and engages the core for stability
Stand upright and keep the back straight. Note: Beginners or those with back issues can perform this exercise seated. Hold a small weight in each hand at the shoulders, with an overhand grip. Thumbs are on the inside and knuckles face up. Exhale as you raise the weights above the head in a controlled motion. Pause briefly at the top of the motion. Inhale and return the weights to your shoulders.
 6. Calf Raises
6. Calf Raises
Benefits: Strengthen lower leg muscles, increase stability, balance and agility
Start by standing 6 to 12 inches away from a wall, facing it, with feet hip width apart. Extend arms to place your palms on the wall, level with chest or shoulders. Exhale and slowly lift heels off the floor, keeping knees extended without rotating your feet. Use your hands on the wall to support your body. Hold raised position briefly. Inhale and slowly lower heels back to the floor.
 7. Plank Pose
7. Plank Pose
Benefits: Strengthens the core and abdominals while increasing stability and balance
Modified version: Start in tabletop position with hands and knees on the floor. Walk your hands so your forearms and palms are facing down, keep shoulders and elbows aligned. Walk your knees away from your body until you feel your core and abdominals engaged. Keep torso straight and rigid, your body in a straight line from ears to knees with no sagging or bending, and with shoulders down, not creeping up toward your ears. You may keep your toes on the floor for extra support. Hold position for 10 seconds. Walk your knees back in, repeat. Over time, work up to 30, 45 or 60 seconds.
Sources/refer to these websites for more detailed descriptions on the exercises: American Council on Exercise, Verywell Fit, Women’s Health
*As President and Chief Science Officer at the American Council on Exercise, Cedric X. Bryant, PH.D and Fellow of the American College of Sports Medicine, stewards the organization’s exercise-science and behavior-change education. He earned both his doctorate in physiology and master’s degree in exercise science from Pennsylvania State University, where he received the Penn State Alumni Fellow Award, the school’s highest alumni honor.
by Specialdocs Consultants | Apr 1, 2022 | Medical Conditions, Patient News, Wellness
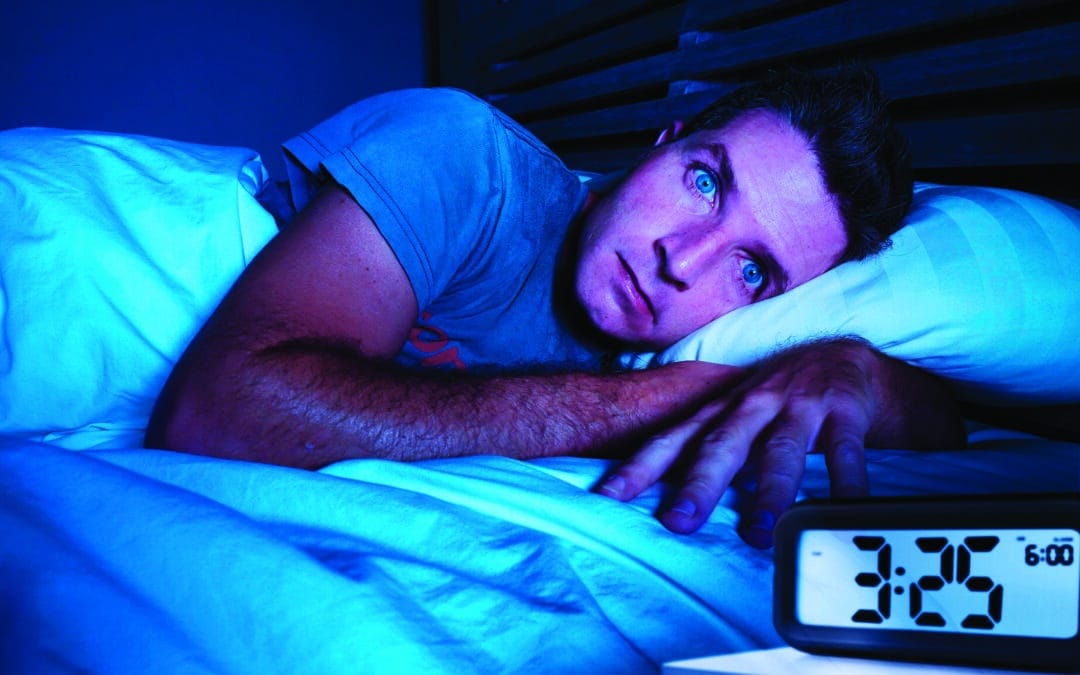
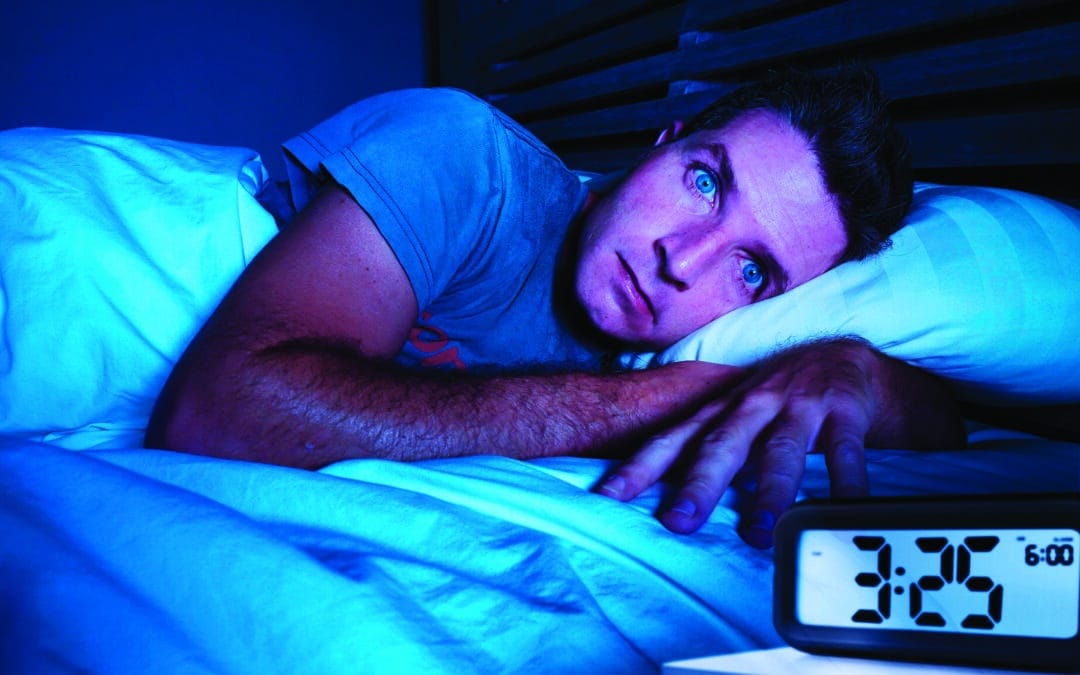
Breaking the Cycle of Anxiety, Insomnia and Sleep Anxiety
A good night’s sleep does more than refresh and revitalize. It’s essential to your health, so make it a priority to understand what’s keeping you up at night.
“Healthy sleep is as important as proper nutrition and regular exercise for our physical and mental well-being,” says Kannan Ramar, MD, sleep medicine physician at the Mayo Clinic’s Center for Sleep Medicine and immediate past president of the American Academy of Sleep Medicine. “Lack of sufficient sleep is associated with increased risks of type 2 diabetes, high blood pressure, cardiovascular disease, depression and anxiety.”
The sleepless nights and drowsy days previously experienced by one out of three Americans with insomnia rose to pandemic highs of almost 60% in 2021, sounding a wake-up call to address this treatable condition which profoundly impacts both mental and physical well-being.
Sleep disturbance is intricately interconnected with the presence of issues such as anxiety and depression, each influencing the others, so it’s not always possible to determine which came first. Behavioral changes that result from chronic insomnia include feelings of being overwhelmed, inability to concentrate, irritability, nervousness, restlessness, and a sense of impending danger or doom.
Of adults diagnosed with depression, 75% experience insomnia and 20% have obstructive sleep apnea. Similarly, anxiety can make it harder for the body to relax and fall asleep.
Research suggests that anxiety can also affect rapid eye movement (REM) during slumber and trigger vivid, disturbing dreams that wake the sleeper.
Completing the loop is sleep anxiety — apprehension or fear about going to sleep — which is commonly seen in those with insomnia, narcolepsy, sleep apnea or restless legs syndrome.
While insomnia can seem never-ending, a number of strategies can effectively break the cycle.
The Basics:
- Set boundaries for blue light exposure by turning off tv, tablets and phones at least 30 minutes before bedtime.
- Limit large meals, caffeine and alcohol within 3 to 4 hours of bedtime, which can disrupt sleep. Alcohol allows you to fall asleep quickly but not stay asleep throughout the night.
- Establish a consistent wake-up time seven days a week.
- Ensure your bedroom is a designated place of sleep by keeping it dark, cool and quiet. And turn around your clock so you can’t see the time if you’re tossing and turning in the middle of the night.
- Pursue support if you are experiencing chronic insomnia, defined as difficulty sleeping three or more times per week for at least three months. “We know that the longer insomnia lasts, the more difficult it is to treat,” says Dr. Ramar.
Support can include:
- Cognitive behavioral therapy for insomnia (CBTI), a form of talk therapy focused on learning how to create an optimal sleep environment with positive bedtime routines and avoidance of factors that trigger anxiety and negative thinking. Requiring up to 12 weeks to see results, the key is shifting from “trying hard to sleep” to “allowing sleep to happen,” according to Stanford Health.
- Prescription sleep hypnotics, such as Ambien or Lunesta. Hypnotics can be considered in conjunction with CBTI, but patients must be closely monitored for adverse effects and a buildup of tolerance to the medication’s effects. Low doses of Trazodone, an antidepressant, are sometimes used, as it causes drowsiness.
- Light therapy, which is especially helpful for those who need to reset their circadian rhythms; e.g., a night owl who wants to function better with an early morning rising time.
If you are experiencing too many wakeful nights, please let your healthcare provider know. It may be helpful to keep a sleep diary for several weeks to help pinpoint the habits affecting your ability to fall and stay asleep. In some cases, we may recommend a polysomnography (sleep study), where you’ll be monitored for blood oxygen levels, body position, breathing, electrical activity in the brain, eye and leg movements, heart rates and rhythms, sleep stages and snoring during an overnight stay in a sleep lab.
Finally, keep in mind that the amount of sleep needed per night – typically 7 or 8 hours on average – varies by individual. “If you function well and are fully alert during the day, you can be confident your sleep needs are being met,” says Dr. Ramar.

by Specialdocs Consultants | Apr 1, 2022 | Medical Tests, Patient News, Staying Active, Wellness
Definitive Diagnostic Tool or Part of a Greater Health Matrix?
It’s an easily understood calculation: Body Mass Index, popularly known as BMI, computes an individual’s measure of body fat as weight in kilograms divided by height in meters squared. Levels are defined as Underweight if less than 18.5, Normal weight if between 18.5 and 24.9, Overweight if between 25.0 and 29.9, and Obese if above 30. But what does BMI really tell us?
This simple formula has nonetheless sparked controversy and continued questioning: Is BMI a quick, easy and efficient way to identify weight problems and associated risk of disease in adults? Or is it an inaccurate measure because it doesn’t consider body composition, age, sex or ethnicity?
Years of debate, research and analysis now point to using BMI in a more nuanced way, suggesting that it is best employed as just one part of an initial health screening for individuals, and not as a diagnostic tool. Much more meaningful is how BMI fits with other essential measures of an individual’s health — blood pressure, blood sugar, cholesterol levels, heart rate, inflammation, physical activity, diet, cigarette smoking and family history.
Looking at BMI alone can be misleading when you consider that:
- Women tend to have more body fat than men.
- Older adults have more body fat than younger ones. Aging is associated with an unhealthy increase in body fat and an associated increased risk for prediabetes and type 2 diabetes.
- At the same BMI, the metabolic risks for people of Asian descent are higher than for Caucasians.
- People who engage in strength training two or more times per week have higher lean muscle mass than nonathletes, which can result in a higher BMI but not necessarily a higher risk of disease.
Additionally, knowing where the fat is distributed is essential in determining disease risk. The pear shape associated with women means subcutaneous fat around the hips, thighs and buttocks; more dangerous is the apple shape, which indicates visceral fat in the abdomen (waist circumference of more than 40 inches for men or more than 35 inches for nonpregnant women), which is linked to higher risk of heart disease and type 2 diabetes.
An influential study published in Nature further revealed the flaws in categorizing people as “unhealthy” or “healthy” based on BMI alone. The authors found that more than 74 million American adults were miscategorized. Nearly half of people considered overweight and 29% of those categorized as obese were actually metabolically healthy, with normal blood pressure, cholesterol and blood glucose levels. Meanwhile, 30% of those considered “normal weight” had metabolic or heart issues.
The origins of BMI help explain its limitations. In the 1830s Belgian mathematician Lambert Adolphe Jacques Quetelet developed a test intended to identify the “l’homme moyen,” or the “average man,” by taking the measurements of thousands of Western European men and comparing them to find the ideal weight. More than a century later, American physiologist and dietician Ancel Keys promoted Quetelet’s Index as the best available way to quickly screen for obesity, identifying certain BMI ranges as associated with greater risk of disease and poor health outcomes. However, like Quetelet, Keys didn’t account for different body types or ethnicities.
One other point to consider: While more intrusive and not as commonly available, methods such as measuring skinfold thicknesses, bioelectrical impedance, underwater weighing, abdominal CT scans (for visceral fat) and dual-energy X-ray absorption are more accurate than BMI for estimating body fat.
So is BMI still meaningful?
As a discussion point, or as one tool used in combination with other assessments of metabolic and skeletal health, it can be useful.
Most importantly, body fat is just one of many factors considered when evaluating individual health and risk of disease.
We encourage you to call your healthcare provider to discuss your personal wellness profile.





 1.
1.  2.
2.  3.
3.  4.
4.  5.
5.  6.
6.  7.
7. 

Recent Comments