by Ivan | May 1, 2020 | Nutrition, Patient News


Nutrition Health Spotlight: Kombucha, Kimchi and More
Researchers continue to examine the trillions of bacterial species residing in our gut microbiome to better understand their potential to help maintain health and prevent disease. Some of the most studied are probiotics, microorganisms found in yogurt and other fermented items. Probiotic foods are much in demand as a tasty, trendy way to improve “good” bacteria and enhance digestive health…but can they? We’ll find out in this Nutrition Health Spotlight.
The landscape is a confusing one, spawning a multimillion-dollar industry of probiotic-rich foods and supplements and a growing fascination with fermentation. But keep these facts in mind: No health claims for probiotics have yet been approved by the Food and Drug Administration, and, overall, data is still emerging regarding the potential health benefits of fermented foods. We checked in with Robert Hutkins, Ph.D., professor of food science at the University of Nebraska, who literally wrote the book on the topic with the second edition of Microbiology and Technology of Fermented Foods.
Q: What sparked the newfound popularity of centuries-old fermented foods?
A: When I wrote the first edition of the textbook in the early 2000s, fermentation was considered an old science with not much new to be learned. But a perfect storm occurred in the last 10 years, with rising interest in nutrition and health; artisanal, organic and ethnic foods; and bold, unique flavors. All are found in fermented foods. In addition, advances in genome sciences provided researchers with tools to study relevant microbes and microbial communities in nearly every category.
Q: How are fermented foods made?
A: The traditional way is to rely on the microbes already present in that food, as in sauerkraut or kimchi. The other way is to use a starter culture, a concentrated collection of microbes designed to provide consistent flavor and quality, which is how yogurt, cheeses and yeast breads are made. Ultimately, the microbes feed on the starch and sugars in the food to produce lactic acid or ethanol, which have natural antimicrobial activities to protect from spoilage microbes. Nearly every civilization has at least one fermented food as part of its heritage, such as Japanese natto, Hawaiian poi and the Indian yogurt drink lassi.
Q: Why are fermented foods considered healthier?
A: Many fermented foods are rich in live microorganisms, and yogurt, kefir and other products often contain added probiotic microbes known to support a healthy microbiome. But despite a great deal of information that appears to point toward including fermented foods as part of a good diet, we need more clinical human studies to show specifically how they can improve health.
Q: Do all fermented foods contain probiotics?
A: Although overlap exists, fermented foods don’t always contain probiotics. Only specific live microbes that have been identified as having potential health benefits can be considered probiotics, and there are dozens in foods yet to be studied. Another important distinction is that while fermented foods are always made with microorganisms, when processed by baking, smoking or pasteurization, those live microbes are killed. For example, live cultures are present in sourdough bread, but they don’t survive the baking process; likewise for products that are processed, like canned sauerkraut. Also note there are foods that may seem fermented but are not, such as California olives and most pickles, which are simply put into a brine.
Q: I’d like to try adding some fermented foods to my diet. What would you recommend?
A: You’re likely already familiar with yogurt or plant milks that contain live strains of bacteria. Other fermented foods include kefir (a tangy dairy drink), kimchi (a spicy Korean dish of cabbage, radish and scallions), miso (a Japanese fermented soybean paste used in soups and sauces), kombucha (a sweet tea beverage fermented with a symbiotic colony of bacteria and yeast), and cheddar and most other hard cheeses. Many contain healthy omega-3 fatty acids and B vitamins as well as live microbes.
Note: If you are immune compromised, check with our office first about eating unpasteurized fermented foods, like raw milk cheese or dry fermented sausage.
The post Kombucha, Kimchi and More: Nutrition Spotlight appeared first on Specialdocs Consultants.
The post Kombucha, Kimchi and More appeared first on Specialdocs Consultants.
by Ivan | Apr 1, 2020 | Patient News, Wellness

Unleashed: The Healing Power of Dogs
“Who rescued whom?”
They’re already considered best friends, trusty companions and beloved members of the family. Now add to the dog’s list of accomplishments, heart healer, exercise coach, and mood enhancer, and the answer to the question above, often used by rescue organizations, becomes even more meaningful. There is new a body of research that goes beyond the anecdotal charms of dog ownership to provide some increased evidence around the health benefits of pet therapy.
 The impact on patients with cardiovascular disease (CVD) was initially noted by the American Heart Association in 2013 after an examination of studies reporting beneficial effects of dog ownership, including increased physical activity, favorable lipid profiles, lower systemic blood pressure and stress levels, and improved survival after a heart attack. The AHA’s measured conclusion then was that dog ownership “may be reasonable for reduction in CVD risk,” and further research was recommended.
The impact on patients with cardiovascular disease (CVD) was initially noted by the American Heart Association in 2013 after an examination of studies reporting beneficial effects of dog ownership, including increased physical activity, favorable lipid profiles, lower systemic blood pressure and stress levels, and improved survival after a heart attack. The AHA’s measured conclusion then was that dog ownership “may be reasonable for reduction in CVD risk,” and further research was recommended.
Studies show the dog ownership can have healing powers
Late in 2019, a meta-analysis of studies, including data from 3.8 million patients, further bolstered the concept that dog ownership can play a significant role in reducing CVD risk factors by alleviating social isolation, improving physical activity and lowering blood pressure. According to the study, compared to non-owners, dog owners experienced a 24% reduced risk in all-cause mortality, 31% reduction in mortality due to cardiovascular-related issues and 65% reduced risk of mortality after a heart attack.
The AHA noted that while the non-randomized studies can’t conclusively “prove” that owning a dog leads directly to reduced mortality among heart attack and stroke survivors, “the robust findings are certainly suggestive of this” and set the stage for additional exploration.
“The results were very positive,” affirmed researcher Caroline Kramer, MD. “The next step would be an interventional study to evaluate cardiovascular outcomes after adopting a dog and the social and psychological benefits of dog ownership.”
A dog owner herself, she added, “Adopting Romeo [her miniature Schnauzer] has increased my steps and physical activity each day, and filled my daily routine with joy and unconditional love.”
Pet ownership is a long term commitment
As compelling as the statistics are, researchers emphasize that dog adoption should never be done for the primary purpose of reducing CVD risk. The long-term commitment and lifestyle changes involved in dog ownership must be fully understood and accepted.
Consider these questions:
• Do I have time to care for and clean up after the dog?
• What type of environment does the dog need to thrive?
• How large will the dog get and how much exercise will it need?
• What is the dog’s life span, and can I commit to caring for it throughout its life?
• How much will veterinary care cost?
Animal-assisted therapy
The healing power of dogs extends well beyond the home as their value in helping decrease pain, stress and anxiety and aid recovery in people coping with a range of health problems is increasingly recognized. Therapy dogs provide comfort to nursing home residents, hospice patients, prisoners, children coping with trauma, and veterans suffering from post-traumatic stress disorder (PTSD), among others. The field of animal-assisted therapy is growing rapidly, as seen in the success of Mayo Clinic’s Caring Canines program, now in its 10th year. More than a dozen registered therapy dogs make their daily “rounds” of hospital rooms and clinic waiting areas.
“If someone is struggling with something, dogs know how to sit there and be loving,” researcher Dr. Ann Berger explained in the National Institute of Health News. “Their attention is focused on the person all the time.”
The post Pet Therapy: The Healing Power of Dogs appeared first on Specialdocs Consultants.
The post Pet Therapy: The Healing Power of Dogs appeared first on Specialdocs Consultants.
by Ivan | Mar 1, 2020 | Nutrition, Patient News

Examining Plant Based Burgers as Meat Alternatives
They’re 2019’s most sizzling success story, found everywhere from grocery freezer to fast food counter. Impossible Foods and Beyond Meat have brought plant based burgers from fringe to mainstream with remarkable rapidity. So quickly, in fact, that despite their ubiquity, questions abound regarding the burgers’ benefits. What exactly are they made of? Are they flavorful? How do they compare nutritionally with a turkey patty or an all-beef quarter pounder? Are they meant for a healthy planet and a healthy body?
Both feature a lengthy list of ingredients that may seem far from natural, but both plant based burgers were formulated to recreate the meaty, juicy mouthfeel of a hamburger. That being said, hundreds of meat alternative taste tests and rave reviews have demonstrated that expectations have indeed, been exceeded.
Ironically, many vegans haven’t embraced these plant-based burgers precisely because their taste, smell and texture evokes a beefy authenticity they’ve long eschewed.
What Goes Into Plant Based Burgers?
Impossible Burger is made primarily of soy protein concentrate, coconut and sunflower oil, binders, vitamins, minerals and the key ingredient – soy leghemoglobin, or “heme” – which makes the burger “bleed” and brown like meat. Beyond Burger, recently reconfigured to promise an even meatier flavor and chew, features an elaborate combination of plant proteins including pea and mung bean; fats for cooking sizzle, such as coconut oil and cocoa butter; minerals like calcium and iron; potato starch to bind; and beet juice extract for a beef-like red color in their plant based burgers.
Just the (nutritional) Facts!
Nutritional info for plant based burgers, paints a somewhat mixed picture. The good news is, the burgers contain approximately 20 grams of protein (equivalent to ground beef); a healthy mix of vitamins and minerals, including B vitamin, zinc and iron; and no cholesterol.
Interestingly, the plant based burgers may not be the best choice for people following a heart-healthy diet, as they are higher in saturated fat than turkey burgers and contain substantially more sodium than lean beef burgers. Moreover, you might consider creating your own vegetarian burger with beans, whole grains, herbs, seeds and nuts as a healthier option.
“These burgers offer good amounts of antioxidants and certain vitamins and minerals, but they aren’t quite the same as a whole-foods veggie burger made from beans,” explains Registered Dietitian Ginger Hultin, spokesperson for the Academy of Nutrition and Dietetics. “In order to mimic meat well, they use a blend of ingredients that includes saturated fat, similar to a beef burger, but from coconut oil.”
So, what’s the verdict?
“They’re interesting, delicious products that can fit into a balanced diet, and have benefits in the form of supporting the environment and saving the lives of animals,” she says.
| 4 oz. portion |
Impossible Burger |
Beyond Burger |
85% lean burger |
90% lean burger |
Turkey burger |
| Total Fat |
14g |
18 g |
15 g |
10 g |
10 g |
| Sat. Fat |
8 g |
6 g |
6 g |
4 g |
3 g |
| Cholesterol |
0 mg |
o mg |
88 mg |
65 mg |
92 mg |
| Sodium |
370 mg |
390 mg |
72 mg |
66 mg |
400 mg |
To sum up, supporting the environment and saving the lives of Animals is, in fact, the real fuel driving these companies, both of which are on a mission to reduce meat consumption and ensure a sustainable global food supply by giving people what they enjoy most – big, juicy (plant based) burgers.
The post Are Plant Based Burgers Really Healthier? appeared first on Specialdocs Consultants.
by Specialdocs Consultants, LLC | Feb 1, 2020 | Medical Conditions, Patient News

Oh, My Aching Head
A dull pressure, a sharp pain, an uncomfortable pounding, a vise-like sensation – all can signal the start of a headache. A painful part of the human condition since the beginning of time, more than 150 different types of headaches have been identified, categorized and treated in increasingly effective ways. We take a look at how to cope with the most common headaches, as well as when your symptoms indicate immediate attention is needed in this great reference guide to headache types and remedies.
 Tension Headache
Tension Headache
It’s the rare person who hasn’t experienced the tight feeling or band-like grip around the head that characterizes a tension headache. Stress is frequently the trigger, so staving them off with recognized stress management strategies such as deep breathing exercises, yoga, meditation, and progressive muscle relaxation may help. For immediate relief, gentle massage and use of warmth or heat to ease tense neck and shoulder muscles often work well. Over-the-counter medicine such as aspirin, ibuprofen or acetaminophen may also be used judiciously.
Cluster Headache
Seen more often in men, these headaches cause intense pain on one side of the head or around one eye; are often accompanied by nasal discharge or teary eyes; and occur in bouts of frequent attacks over weeks or months, followed by long periods of remission. Treatments include inhaling pure oxygen through a face mask, which often relieves pain within 15 minutes, and injectable triptan medications used to treat migraines.
Exertional Headache
Headaches experienced after strenuous exercise may result from being dehydrated or overheated or simply from overexertion, and are usually resolved quickly with rest and adequate hydration.
Sinus Headache
The pain, pressure and fullness in cheeks, brow or forehead, often accompanied by stuffy nose, fatigue and an upper toothache, can indicate a headache from sinusitis or seasonal allergies, but be aware that in many cases it is actually a migraine. Rest, fluids, decongestants and over-the-counter pain medications help alleviate headaches caused by sinusitis; those caused by an allergy will usually be treated with a nasal spray.
Each headache has its own “flavor,” but if they occur more frequently or more severely, seem to worsen with the use of over-the-counter drugs, and interfere with your normal activities, please contact us…and consider starting a headache journal that you can bring to your appointment. Track if they are occurring at certain times of day, or after specific activities or foods; e.g., after a workout, a sleepless night or a change in diet. Also note the duration of each headache; where the pain is located; the intensity and type of pain; other accompanying symptoms, such as gastrointestinal distress; and medications you used. Pre-formatted trackers can be accessed online at sites such as headaches.org.
When to seek help promptly: If your headache can be described as one of the worst you’ve ever experienced and is accompanied by trouble seeing, speaking or walking; fainting; high fever; numbness, weakness or paralysis on one side of your body; stiff neck; or nausea or vomiting.
Inside the ‘Migraine Brain’
Despite the prevalence of migraine headaches, which affect 39 million people in the U.S. alone, their complex and multifactorial causes have made it difficult to pinpoint the most effective management of often debilitating symptoms that can include severe, pulsating pain; nausea; and visual auras. But years of research into the “migraine brain” are revealing a deeper understanding and new treatments, discussed in our Q&A with a headache expert, below.
Q: What is a migraine brain?
A: We have found it’s wired somewhat differently than the average brain, highly sensitive to light, sound and movement.
Q: Does genetics play a role?
A: Absolutely, as more than 70% of migraine sufferers have at least one close relative with the problem.
Q: What triggers a migraine?
A: Among the multiple factors are stress, hormonal shifts, time and travel changes, certain foods, inadequate nutrition, alcohol, and too much or too little caffeine. Anyone of these, or more likely, a combination, can trigger an episode. But the number one cause is the overuse of migraine medications, which triggers rebound headaches and starts a cycle of needing increasing quantities for relief.
Q: What medications are used to manage or prevent symptoms?
A: In addition to over-the-counter medications such as acetaminophen, a class of drugs called triptans that block pain signals in the brain have been used effectively for years. There are many other options, such as new biologic drugs to prevent or minimize the pain of migraines, including calcitonin gene-related peptide (CGRP) inhibitors and serotonin-receptor agonists.
Q: Will lifestyle adjustments make a difference?
A: There is no question that migraine patients benefit most from a set routine of healthy eating (avoiding alcohol and foods with nitrites or preservatives) and regular exercise; getting adequate sleep each night; and learning to manage stress with techniques such as biofeedback training, relaxation training and cognitive-behavioral therapy.
The post Headaches – Types and Remedies appeared first on Specialdocs Consultants.
by Ivan | Jan 16, 2020 | Medications, Patient News

Antibiotics Awareness
Spurred by Alexander Fleming’s serendipitous discovery of penicillin in 1928, antibiotics have rightfully become wonder drugs, often able to change the course of deadly bacterial infections in a matter of days. But in recent years, their unmatched healing power has become overprescribed and over utilized, leading to concerning findings like these: Nearly 23% of antibiotic prescriptions filled in 2016 were unnecessary, and an additional 36% were prescribed for conditions for which an antibiotic is only sometimes recommended, according to a recent study from the Agency for Healthcare Research and Quality. Antibiotics awareness is good for your health
Unintended consequences far from benign
Patients may needlessly experience the drug’s side effects, such as rash, dizziness, nausea, diarrhea or Clostridium difficile infection (C. diff), which can cause severe diarrhea and may be life-threatening. On a larger, global scale, overuse leads to antibiotic-resistant bacteria, a growing danger that occurs when bacteria that have been exposed to an antibiotic mutate, rendering the drug ineffective against them. The Centers for Disease Control estimates that at least 2 million people are infected with antibiotic-resistant bacteria each year in the US, resulting in approximately 23,000 deaths. In fact, Fleming himself predicted the possibility in his 1945 Nobel Prize acceptance speech, saying: “It is not difficult to make microbes resistant to penicillin in the laboratory by exposing them to concentrations not sufficient to kill them, and the same thing has occasionally happened in the body.”
Antibiotics: Handle With Care
That’s why the World Health Organization’s annual “Antibiotics: Handle With Care” campaign, launched in 2015, and the United States’ “Be Antibiotics Aware” program, launched the following year, are more important than ever in raising awareness as to why antibiotics aren’t always the answer. Becoming knowledgeable about the difference between bacterial and viral infections, and why an observational (“watch and wait”) approach to antibiotic treatment may be considered for conditions like sinusitis or ear infections, is critical to stemming the tide of overuse.
Below is a look at when antibiotics should be the treatment of choice, when they should be considered only after watching and waiting, or when they are not called for at all. Note that antibiotic drugs effectively kill bacteria but not viruses, which is why they are never recommended for viral infections such as colds or flu. However, not all bacterial infections require the use of antibiotics. As always, check-in with our office regarding what’s best for your individual health.
| CONDITION |
ARE ANTIBIOTICS THE ANSWER? |
SYMPTOM MANAGEMENT |
| Common cold/upper respiratory infection |
No, primarily viral |
Cough expectorants sometimes combined with decongestants; antihistamines; and cough suppressants |
| Flu |
No, primarily viral |
Antiviral drugs by prescription |
| Bronchitis/chest cold |
No, primarily viral; thick, yellow or green mucus does not indicate bacterial infection |
Cough suppressants/expectorants; decongestants; antihistamines |
| Sore throat |
Only if diagnosed with group A streptococcal pharyngitis (the cause of just 5-10% of adult sore throats) |
Over-the-counter (OTC) pain relievers such as aspirin, ibuprofen and acetaminophen; throat lozenges |
| Sinusitis |
Only if severe, or if symptoms persist after
10-14 days. Many studies show no difference in recovery rate with or without antibiotics.
Sinusitis infections are primarily viral; even if diagnosed as bacterial, a watch and wait approach may be recommended. |
OTC pain relievers |
| Pneumonia |
Yes, if diagnosed as bacterial |
OTC fever reducers/pain relievers |
| Middle ear infection |
For mild cases, watchful waiting or delayed antibiotic prescribing may be recommended |
Extra fluids; OTC pain relievers |
| Cystitis, a common bladder infection in females |
Yes, this infection is usually bacterial |
Fluids; heating pad on lower abdomen; warm bath |
| Lyme disease |
Yes, cause is a bacteria transmitted to humans by a bite from an infected tick; treatment with antibiotics in early stages of disease is most effective and prevents later-stage complications |
|
Sources: Up to Date, CDC
About that penicillin allergy
Most people who believe they’re allergic to penicillin can take it without a problem, either because of the rash, they experienced as part of a virus or because the allergy resolved over time. You may want to get tested by an allergist to be certain, as research shows that patients identified as penicillin-allergic are more likely to receive very powerful antibiotics with greater side effects, and are also at higher risk of developing resistant infections that require longer stays in the hospital. It’s interesting to note that when skin tested, approximately 90% of people will test negative for a penicillin allergy.
Did You Know?
Reactions from antibiotics cause 1 out of 5 medication-related visits to the emergency department.
Source: Centers for Disease Control
The post Antibiotics Awareness is Good for Your Health appeared first on Specialdocs Consultants.
by Ivan | Dec 2, 2019 | Medical Conditions, Patient News, Wellness
The Female Factor: Alcohol is Not Gender-Neutral
Given the growing popularity of the cocktail culture and wine time, it’s important to know that alcohol affects women differently than men – physiologically, psychologically and socially. It’s worth asking: For women, is the wine glass half full or half empty when considering the risk-versus-benefit ratio?
First, there is the difference in women’s body composition. Women have more total body fat and less total body water than men. As a result, alcohol is less dispersed, resulting in a higher blood alcohol level, drink for drink, than in men.
Metabolism also plays a role
Women produce less of the alcohol dehydrogenase (ADH) enzyme that controls the rate at which alcohol is broken down in the body. This means a blood alcohol level that rises more quickly in women and stays elevated longer. Women are more vulnerable than men to alcohol’s effects on other levels too: more likely to black out from drinking, to suffer from mood and behavioral changes and to more rapidly develop an addiction. Women may also experience higher rates of depression and anxiety, often drinking in response to negative emotions and problems with loved ones versus men’s tendency to drink for positive reinforcement and pleasure.
High Drinking Rates in Women: A Cause for Concern
All these factors make the record high drinking rates for women a real cause for concern. Problem drinking rose by 83% among women from 2002 to 2013, rapidly closing – in a most unfortunate way – a gender gap that has existed for decades. Current statistics show that 5.4 million women over 18 may be considered as having alcohol use disorder (AUD) and need treatment. However, gender plays a role here too, as women who consistently seek treatment for almost every other physical and mental health problem at higher rates than men are far less likely to do so for alcohol-related problems. Less than 1 in 10 women get formal help, hindered by the stigma of addiction and feelings of guilt or shame in not being able to function as caregiver for their family.
Alcohol’s impact on other disease is mixed. There is evidence that one drink a day may reduce women’s risk of heart attack, cardiovascular disease and the most common type of stroke. The risk of breast cancer, however, increases by 5 – 9% and rises with each additional drink per day. It’s worth noting that taking a multivitamin fortified with 400 mcg of folic acid daily may lower some of women’s elevated risk from alcohol, according to recent studies.
Alcohol in Moderation is Key
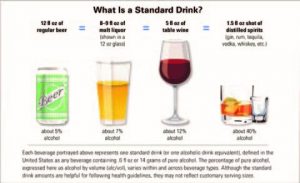
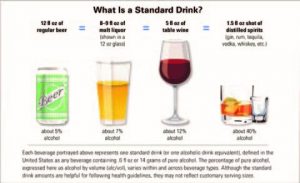
The best advice, as with most of life’s issues, is moderation. Avoid alcohol if pregnant or if you have a personal or family history of breast cancer, liver disease or alcohol abuse. Otherwise, consuming one drink a day is generally healthy, so be knowledgeable about how to measure that (see below) and enjoy a glass with friends or at special events. Don’t try to match the pace of male celebrants, especially if they’re over-imbibing. In fact, gently steering them away from the bar and onto the dance floor may be the healthiest move for all.
Heavy drinking for women = more than one drink per day or seven-plus drinks per week
Did You Know?
Alcohol use disorder is characterized by symptoms such as:
· excessive time spent drinking
· needing to drink more to get the same effect
· wanting a drink so badly you can’t think of anything else
· inability to stop drinking despite the impact on work and family
*Source: National Institute on Alcohol Abuse and Alcoholism
The post Alcohol Affects Women Differently than Men appeared first on Specialdocs Consultants.




 The impact on patients with cardiovascular disease (CVD) was initially noted by the American Heart Association in 2013 after an examination of studies reporting beneficial effects of dog ownership, including increased physical activity, favorable lipid profiles, lower systemic blood pressure and stress levels, and improved survival after a heart attack. The AHA’s measured conclusion then was that dog ownership “may be reasonable for reduction in CVD risk,” and further research was recommended.
The impact on patients with cardiovascular disease (CVD) was initially noted by the American Heart Association in 2013 after an examination of studies reporting beneficial effects of dog ownership, including increased physical activity, favorable lipid profiles, lower systemic blood pressure and stress levels, and improved survival after a heart attack. The AHA’s measured conclusion then was that dog ownership “may be reasonable for reduction in CVD risk,” and further research was recommended.


Recent Comments