
by Specialdocs Consultants | Jul 11, 2023 | Medications, Patient News
For patients seeking new solutions to managing type 2 diabetes and obesity, the introduction of a class of drugs called GLP-1 receptor agonists (RA) has simultaneously inspired hope and excitement along with misuse and confusion. We developed the following Q&A to go beyond the headlines and explore how Ozempic and similar drugs work, who may benefit most from them, and why they may ultimately represent a true breakthrough in the way these chronic conditions are classified, considered and treated.
What defines type 2 diabetes?
More than 37 million Americans have type 2 diabetes, a chronic disease that affects the ability of the body to regulate glucose (blood sugar) levels. This leads to an increase of glucose over
time which significantly increases the risk for complications to vital organs such as the heart, kidneys, eyes and nerves. Diagnosis is made when testing shows: fasting glucose of 126 mg/dl or higher; or non-fasting glucose of 200 mg/dl or higher; or A1C (average of glucose over the past 3 months) of 6.5% or higher.
How was type 2 diabetes previously treated?
Approved by the FDA in 1994, Metformin is well established as the first line therapy for management of type 2 diabetes if lifestyle changes (low-carbohydrate diet, weight loss and exercise activity) are not enough to bring blood sugar levels down near the normal range. Metformin works by decreasing the amount of blood sugar produced by the liver in a fasting state, decreasing the absorption of food through the intestines, and restoring the body’s response to insulin.
What is different about the GLP-1 RA drugs?
Among the major benefits this class of drugs brings to patients with type 2 diabetes is
lowering their risk for heart disease and stroke, and providing a significant boost to weight loss, in addition to helping reduce glucose levels to a near-normal range. As a result of the positive outcome reported in trials, the American Diabetes Association changed its longstanding guidelines for first-line treatment of type 2 diabetes to include recommendations for GLP-1 RA drugs in patients at high risk for cardiovascular disease or with risk factors such as high blood pressure, high cholesterol, or chronic kidney disease.
How do GLP-1 RA drugs work?
Known as incretin mimetics, this class of drugs mimics the effect of a hormone, glucagon- like peptide-1, or GLP-1, which is normally produced naturally to stimulate the release of insulin secretion after eating a meal. Receptors to GLP-1 are found in the pancreas, the brain and elsewhere in the body. The drug enhances these receptors, which help the pancreas release more insulin and help reduce blood sugar levels without raising the risk for hypoglycemia (too- low blood sugar levels). By limiting the amount of sugar the liver releases into the bloodstream in a fasting state, and slowing down how long food stays in the stomach, the drug promotes a feeling of satiety, leading people to be satisfied with eating smaller portions. In addition, some patients have reported a marked decrease in cravings for carbohydrate-rich and fatty foods.
What are GLP-1 RA drugs intended to treat – diabetes, obesity, or both?
Under certain names, GLP-1 RA drugs are FDA-approved only for treatment of type 2 diabetes while offering added benefits of weight loss and cardiovascular protection; under other names, the drugs are indicated only for weight loss, but not for treatment of diabetes. While the ingredients can be identical, the difference is in dosage amounts and whether the trials focused on the drug’s impact on blood sugar or weight changes. For example, semaglutide, a GLP-1 drug, is approved to treat diabetes under the name Ozempic; a higher-dose version of semaglutide, Wegovy, is only FDA approved for weight loss. The same is true for liragutide, approved for type 2 diabetes as Victoza, and for weight loss as Saxenda.
Are there side effects?
Most side effects for these types on drugs are gastrointestinal, including nausea, diarrhea or constipation, abdominal pain.
How effective are GLP-1 RA drugs like Saxenda and Wegovy for weight loss?
Trials to date have shown excellent results, with patients able to lose between 5 to 20% of their total body weight. However, these drugs are not meant for people wanting to lose 10 or 15 pounds. They are indicated for those who are obese, as measured by a body mass index (BMI) of 30 or higher; or for people with a BMI of 27 or greater with at least one weight-related coexisting condition such as high blood pressure, elevated cholesterol levels. It’s important to note that obesity is a chronic disease, and these drugs may be needed as a long-term treatment to help lose pounds and maintain weight loss, along with lifestyle changes that include a healthy diet and 150 minutes a week of moderate-intensity aerobic and muscle-strengthening activities.
How do SGLT2 inhibitors fit into the mix of drugs for diabetes?
This is a newer class of drugs that lowers blood sugar levels by preventing the kidneys from reabsorbing glucose back into the bloodstream but instead releasing it through urine. Originally intended only for lowering blood sugar, later research data showed the drugs offered significant benefits for type 2 diabetes patients with coexisting conditions. Now some SGLT2 drugs- Invokana (canaglifozin), Farxiga (dapaglifozin), and Jardiance (empagliflozin) – have also been approved for use by non-diabetic patients with a history of chronic kidney disease or congestive heart failure.
Are other drugs in the wings?
Mounjaro, a GLP-1 RA drug that also promotes a second gut hormone (glucose-dependent
insulinotropic polypeptide, or GIP) is currently approved for treatment of type 2 diabetes, and on a fast track approval by the FDA to be used as a weight loss medication.
How will I know which drug is right for me?
This is a decision best made on an individual basis with your physician, who will consider factors such as your overall health status, drug intolerances, risk factors for developing diabetes-related complications, benefits versus possible harm from side effects, and preferred formulation (oral or injection).
Drugs with Benefits: A Guide to GLP-1 RA Therapies
NOTE: Non-GLP-1 RA drugs used for weight loss are not listed here… Please consult with your healthcare provider regarding your best option.
| Brand Name |
Active Ingredient |
Dosage/Form |
Approved For |
Also Beneficial For |
| Ozempic |
Semaglutide |
Weekly injection |
Type 2 diabetes |
Weight loss; decreased risk of stroke and heart attack |
| Wegovy |
Semaglutide |
Weekly injection |
Weight Loss |
n/a, studies not conducted |
| Rybelsus |
Semaglutide |
Daily pill |
Type 2 diabetes |
Weight loss, cardiovascular safety |
| Trulicity |
Dulaglutide |
Weekly injection |
Type 2 diabetes |
Weight loss; decreased risk of stroke and heart attack |
| Victoza |
Liraglutide |
Daily injection |
Type 2 diabetes |
Weight loss; decreased risk of stroke and heart attack |
| Saxenda |
Liraglutide |
Daily injection |
Type 2 diabetes |
n/a, studies not conducted |
| Soliqua |
Insulin glargine & lixisenatide |
Daily injection |
Type 2 diabetes |
Weight loss |
| Byetta |
Exenatide |
Twice daily injection |
Type 2 diabetes |
Weight loss |
| Bydureon BC |
Exenatide |
Weekly injection |
Type 2 diabetes |
Weight loss |
| Mounjaro (GLP-1 RA/GIP) |
Tirzepatide |
Weekly injection |
Type 2 diabetes |
Weight loss |
Sources: GoodRx, American Diabetes Association

by Specialdocs Consultants | Jul 11, 2023 | Patient News, Wellness
Summertime is prime time for ticks, which are becoming more prevalent each year. A combination of changing land use and warmer winters has greatly expanded the ticks’ habitat and they’re now found in more than half of U.S. counties. As a result, tick-borne Lyme disease has doubled over the last two decades to nearly 500,000 cases annually, earning it the unfortunate distinction of being the most common vector-borne illness in the Northern hemisphere. Read on for details on how to protect yourself this season, and in the summers to come.
Identifying Lyme
In its acute phase (one to two weeks after the bite), Lyme can cause fevers and chills, joint pain, headache, muscle aches and is frequently accompanied by a salmon-colored rash at the site of the tick bite. It may have a “bulls-eye” appearance, often considered a sign of infection, but the rash can manifest differently, or not at all. Diagnosis is based on symptoms, physical findings (e.g., rash), the possibility of exposure to infected ticks, and antibody tests. A high number of false negative tests occur in the early phase, however, because it takes time for the immune system to respond to the infection and create antibodies. As the infection progresses, virtually everyone with Lyme disease has a positive test result.
Treating early, late and long Lyme
Most people recover from Lyme disease rapidly and completely if diagnosed early and treated with a short course of oral antibiotics. More serious symptoms, including joint pain and swelling, nerve problems and neurological issues, may develop if Lyme disease is left untreated. Known as late Lyme disease, it can occur months to years after a tick bite, and requires a longer course of antibiotics, administered intravenously. Post-Treatment Lyme disease, sometimes called chronic or long Lyme disease, is experienced by 5% to 15% of patients who have lingering symptoms such as headache, fatigue, joint pain and “brain fog.” While the condition is not yet well understood, experts have found additional antibiotic treatments are not usually helpful, and the symptoms gradually resolve over time.
Preventing Lyme
The best way to avert the complications of Lyme disease is to vigilantly avoid ticks. These tips can help you prevent Lyme disease:
- Wear shoes, long pants tucked into socks, a long-sleeved shirt, hat and gloves in wooded or grassy areas.
- Stick to trails, stay clear of low bushes and long grass.
- Use insect repellants such as DEET, picardin, permethrin (apply to clothing).
- Do tick checks on your body after outside activities. Be sure to check your dogs for ticks
too!
- Remove any ticks promptly with clean, fine-tipped tweezers. Be reassured that just finding a tick on your skin doesn’t mean you’ll get Lyme disease; a tick needs to be attached for at least 48 hours before it can transmit the bacteria.
- Look for advanced protection in the next few years from two well-known names in vaccines – Pfizer and Moderna. An earlier vaccine, LYMERix, was discontinued in 2002 due to lack of interest at a time of lower Lyme disease cases, as well as concerns over side effects. Pfizer’s VLA15 is intended to block the bacteria from leaving the tick. Moderna is applying mRNA technology used in its COVID vaccine to target the Borrelia bacteria species at the root of most U.S. Lyme disease cases. Also of note is MassBiologics’ shot that delivers a single, human anti-Lyme antibody directly to a person to provide immediate immunity…now in trials.
QUICK BITES: Fast Facts About Lyme Disease
- Most Lyme disease infections in the U.S. occur May through September.
- Cases of Lyme disease are most commonly seen in the northeast and mid-Atlantic states
(from Maine to Virginia), the Midwest (Minnesota, Wisconsin, and Michigan), and the
West Coast (California).
- The disease was first recognized in Old Lyme, Connecticut in 1975 when a cluster of
children developed unexplained, rheumatoid arthritis-like symptoms. Not until the next decade was the cause discovered: the spiral bacteria Borrelia burdorferi in deer ticks prevalent in the forests near where the infections occurred. Testing confirmed the Lyme disease bacterium was passed to humans via the bite of a deer tick.
Sources: NIH, National Geographic

by Specialdocs Consultants | Apr 14, 2023 | Healthy Aging, Medications, Nutrition, Patient News
The aching, swollen, stiff joints associated with osteoarthritis (OA) have long been considered a “wear and tear” condition, associated with aging. It was thought that cartilage, the smooth connective tissue on the end of bones that cushion the joints, simply breaks down over a lifetime of walking, exercising and moving. New research shows that it is a disease of the entire joint that also causes bony changes of the joints, deterioration of tendons and ligaments and inflammation of the synovium (lining of the joint). While more prevalent in people over 50, OA can show up in younger patients, especially those who’ve experienced a joint injury such as a torn ACL or meniscus. The promising news is that according to the Arthritis Foundation, “OA is not an inevitable aging disease” and the Cleveland Clinic notes: “Age is a contributing factor, although not all older adults develop osteoarthritis and for those who do, not all develop associated pain.”
Still, currently OA is by far the most prevalent form of arthritis, affecting more than 32.5 million Americans, and primarily targeting knees, hips, hands and spine. A variety of factors contribute to the development of OA, including congenital joint deformity, family history, previous joint injury, and years of physically demanding work or contact sports. However, reducing risk is possible with attention to these modifiable factors:
- Obesity adds stress and pressure to joints. Consider that your knees bear a force equivalent to three to six times your body weight with each step, so a lighter weight relieves the burden considerably – losing one pound takes 3 pounds off the knees.
- Lifestyle. Being physically active is crucial, as a sedentary lifestyle and obesity are associated with a higher risk of OA. While sports such as football, baseball and soccer may pose a risk because of their impact on joints, most types of regular or moderate exercise can be safely done.
Living with Osteoarthritis
Unfortunately, there is no cure for OA, and managing symptoms such as joint stiffness, tenderness, swelling, and popping or crackling can become increasingly difficult over time. While seeking a pill to alleviate discomfort is a natural reaction, consider trying alternative solutions to help break the cycle of chronic pain.
“The longer the brain processes pain, the more hypersensitive it becomes to pain,” explains Rachel Welbel, MD, a physiatrist who is extensively trained in physical medicine and rehabilitation and sports medicine. “The brain, now constantly on high alert, may respond to non-painful sensations as if they are painful. Poor diets and stress can increase chemicals in the brain that reinforce this response, prolonging the pain cycle.”
Reflecting a more holistic and multi-faceted approach to managing pain, she says: “Opioids are almost never the answer.” Instead, she recommends lifestyle modifications, treatments and medications that help tackle pain in a variety of ways.
Lifestyle Modifications, Treatments and Medications for Osteoarthritis
Weight management. Obesity is not only a leading risk factor for OA, but adds to the pain for those with the condition. Body fat produces proteins called cytokines that cause inflammation, and in the joints, can alter the function of cartilage cells. Shedding even a few pounds can make a difference: losing just 10% of your body weight can cut arthritis pain in half, and losing another 20% can reduce the pain by an additional 25% or more, and may slow or even halt progression of the disease.
Exercise and movement. “Exercise is key to living well with OA,” says Welbel. “While resting aching joints may bring temporary relief, lack of movement ultimately leads to more discomfort. The focus is not on weight loss but on minimizing pain and maximizing strength.” Plan on 150 minutes of light to moderate exercise each week. She recommends working with a physical therapist who can analyze your joint biomechanics and suggest exercises to strengthen muscles and improve range of motion while reducing stiffness and pain. “In addition, exercise is a natural mood elevator,” says Welbel. “Walk, swim, or try mindfulness-based, stress-reducing exercise such as yoga and tai chi.”
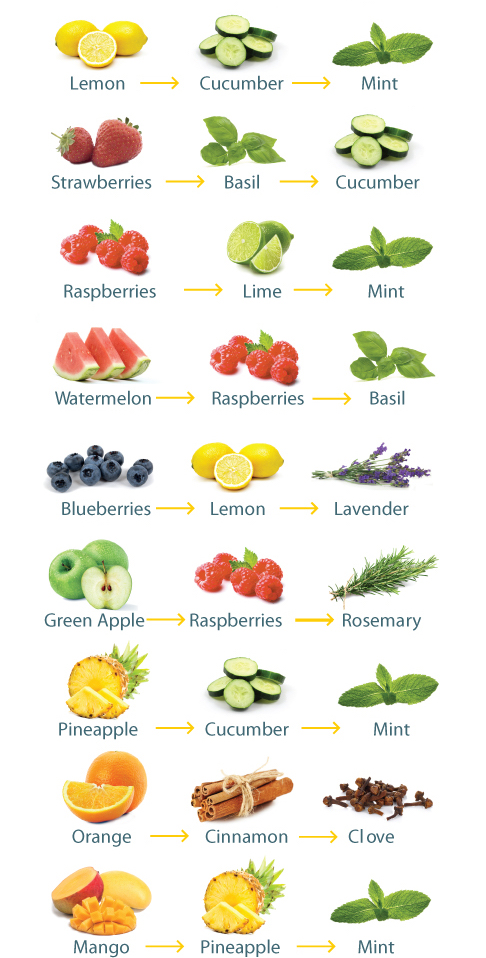
Anti-inflammatory diet. Increasing consumption of fruits, vegetables, whole grains, legumes and fish, while reducing consumption of red and processed meats, refined grains, and sugar-containing beverages and foods, may play an important role in reducing pain associated with inflammation from OA, says Welbel. Try incorporating into your diet fatty fish; herbs and spices such as garlic, turmeric and cinnamon; yogurt and other fermented foods; and healthy fats such as avocados, extra virgin olive oil and walnuts.
Supportive devices. A cane or walker can help lighten the load on your joints, decrease pain, and reduce your risk of falling. Intermittent use of a knee brace may be helpful for added stability, especially if walking on uneven surfaces. Foot orthotics such as arch supports and metatarsal pads may reduce foot pain.
Medications. Over-the-counter (OTC) pain relievers like acetaminophen (Tylenol) may help joint pain and stiffness for some. Nonsteroidal anti-inflammatory drugs (NSAIDs) are also used to relieve pain, including OTC medications such as Advil or Aleve, or Celebrex, a prescription medication with a somewhat lower risk of ulcers and upper gastrointestinal bleeding than other NSAIDs. Topical NSAIDS such as Aspercreme and other creams or patches containing ingredients such as capsaicin, menthol or lidocaine can help.
Injections. Corticosteroids injections may provide temporary relief for acute flare-up of OA pain in knees and finger joints, but effectiveness can vary, and you must wait at least 3 to 6 months to repeat an injection in a specific joint if needed. Viscosupplementation involves injection of a gel-like substance containing hyaluronic acid, which acts as a lubricant in the fluid between bony surfaces and is decreased in OA joints. Research results for significant pain reduction or improved function are not yet convincing, but there appear to be a number of patients with mild to moderate knee OA who report symptom relief.
Supplements. Research results are mixed, but we note some of the more well-known supplements with the caution that these are not recommended to be used alone as treatments for OA. Glucosamine and chondroitin sulfate, naturally occurring compounds found in healthy cartilage, may help reduce joint pain and stiffness, and have been available in the U.S. and Europe for several decades. Other supplements such as tart cherry and turmeric may help reduce OA symptoms for some.
Other promising but not yet proven treatments. Platelet-rich plasma (PRP) injections and stem cell therapy have been used to treat pain of mild to moderate knee OA, but evidence of effectiveness is mixed, and these are still considered experimental. Elements of Eastern medicine, including herbs and acupuncture, may help control OA symptoms, but have not yet been confirmed in large clinical studies.
A Generation of Joint Replacements
When diet and exercise modifications, supportive devices, medications and injections no longer sufficiently ease the pain of OA, a hip or knee replacement may be recommended. The number of people opting for this surgery increases each year, now totaling more than 790,000 knee and 450,000 hip replacements annually.
The implants, made of plastic, metal or ceramic, are traditionally kept in place with bone cement, which is gradually being replaced by newer cementless and porous titanium systems to improve bone fixation and durability. Also on the rise is computer-assisted surgery to increase placement accuracy of the prosthetic components, and patient-specific implants using 3D printing technology. The combination of modern materials and advanced surgical techniques have extended the durability of most implants to 20 years, a marked improvement over the previous standard of 10 to 15 years.
Recovery time has also changed for the better. With rehabilitation to regain strength and motion, normal activities can usually be resumed within weeks to months. Most importantly, the majority of patients are highly satisfied with the results, reporting minimal to no pain and significantly improved function and quality of life. However, outcomes can vary and potential complications should be discussed before proceeding.
Additional breakthroughs may be on the horizon: researchers at Duke University start trials this spring of a hydrogel-based cartilage substitute that may prove more durable than natural cartilage…stay tuned!
Every patient is unique…please check with your healthcare provider to discuss recommendations for prevention and treatment based on your individual health situation.
Sources: Arthritis Foundation, AAOS, Orthoworld, Cleveland Clinic, National Academy of Medicine (formerly Institute of Medicine), UpToDate, US Department of Agriculture, American College of Rheumatology.








Recent Comments